Mile-Markers to Breast Cancer Recovery with SCOUT®: The Tara Zuzga Story
Merit Medical is committed to reducing the burden of breast cancer on patients and their loved ones—patients like Tara Zuzga.

Working in the healthcare industry and having a family history of breast cancer, Tara knew that early detection saves lives. Throughout her life, she diligently underwent regular mammograms and ultrasounds. For a mass like this, however, she couldn’t wait for her next exam. With the support of her husband, who also works in the medical field, Tara connected with Dr. Blumencranz, a breast cancer specialist.
With an accurate diagnosis of breast cancer, she started chemotherapy two weeks later.
AN EXCELLENT CANDIDATE FOR SCOUT®

With Dr. Blumencranz’ help, Tara set off on her journey toward recovery. But she didn’t let her diagnosis slow her down, and she made sure every moment counted.
Tara and her husband continued having special date nights the evening prior to her bi-monthly chemo treatments. “He would take me out just to appreciate that moment before the next morning,” said Tara. “Which was a big deal.”
“She’s like super woman. She’d have her chemo, and then she’d go out walking,” reflected Tara’s husband. “All in all, she was the warrior in all of this.”
YOU’RE NO LONGER MY PATIENT
In January of 2022, Tara received the news she’d been hoping for.
She was cancer-free.
“The day Dr. Blumencranz told me, ‘You’re no longer my patient,’ we both stood there and cried,” said Tara. “When they say we’re checking you out, it’s a really big deal. It’s as big of a deal as ringing the bell for your last chemo. Those mile-markers are everything.”
Watch Tara’s journey to becoming cancer-free.
The Making of Merit Medical—A Timeline Celebrating 35 Years
This year, we’re celebrating 35 years of Merit Medical, an organization founded with a vision to be the most customer-focused company in healthcare. Since then, we’ve expanded from our headquarters in Salt Lake City, UT, to facilities across the world with a diverse, ever-growing portfolio of products.
As with any great business, we couldn’t have done it alone. Our team is at the heart of what we do. We understand clinician needs and innovate products to meet those needs. We deliver diagnostic and treatment solutions that work. Above all, we help ensure our healthcare partners have what they need to help patients live their best lives.
Let’s look back at some of the pivotal moments that made us Merit.
1987
Our story begins more than three decades ago in an industrial park in Murray, UT. Fred Lampropoulos, Merit’s founder and CEO, brought his idea of a stronger, safer, disposable syringe to life—replacing glass syringes currently used in patient care. In 1988, our first syringe hit the market, paving the way for countless medical innovations to come.
1994
To keep up with an increasing demand for our growing portfolio, we opened our first international location, a manufacturing facility in Galway, Ireland. Today, our Galway team continues to thrive. In 2018, they earned the Medtech Company of the Year award in recognition of their dedication.
This same year, we also saw the opening of Merit Sensor, one of several product divisions that bolster our offerings.
1999
This year marked the opening of our Merit Houston facility. A Center of Excellence, Merit Houston specializes in polymer extrusions and catheter manufacturing.
2000
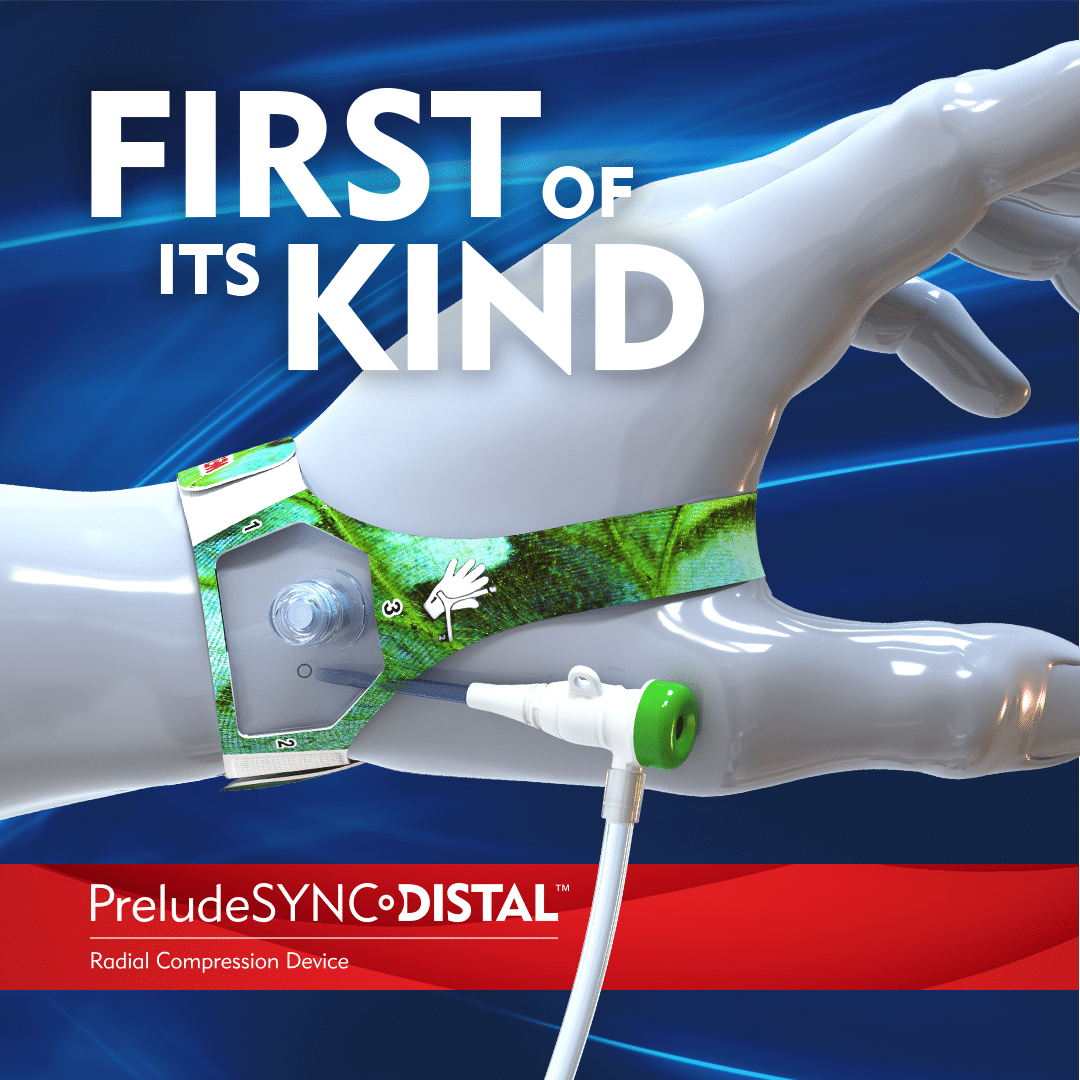
More than a decade of focus and persistence came to fruition in 2000 with the launch of our first compression device, the RADstat® Radial Artery Compression Device. Since then, we’ve continuously innovated and improved our compression device offerings to provide clinicians with superior options—the PreludeSYNC EZ™, PreludeSYNC DISTAL™, and SafeGuard® family of products.
2004
As our US presence continued to grow, we added another location through the acquisition of our Richmond, VA, facility. An integral part of our business, it remains an important manufacturing and distribution center, responsible for producing more than 35 million components each year.
2005
Close to home and far away, this year brought big developments. Our Salt Lake headquarters opened a new manufacturing facility. Doubling its existing square footage, the new facility added more than one hundred new production jobs.
We also opened a facility in Venlo, Netherlands, specializing in manufacturing coated wires, and in 2008, followed with a sister location in Maastricht, our EMEA Distribution Center of Excellence.
2010
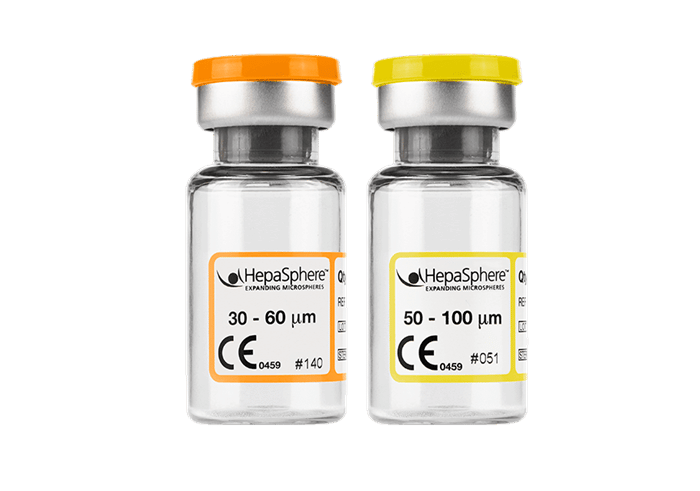
In 2010, we opened our Paris facility. This expansion gave us state-of-the-art embolic material manufacturing capabilities. Our global capacity for delivering more minimally invasive treatment options to patients increased.
2015
Our Tijuana, Mexico, facility opened in 2015, where our dedicated employees enjoy award-winning cafeteria service, a safe and convenient transportation system, and more. As one of our primary manufacturing and assembly facilities, our Tijuana team plays a critical role in our success.
2016
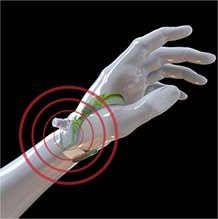
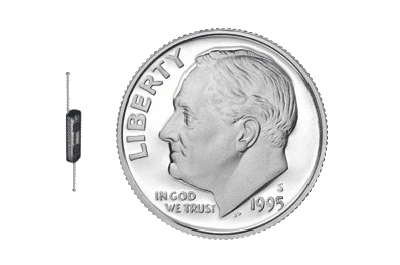
In 2016, we launched the SCOUT® Radar Localization system. Designed to improve patient outcomes, SCOUT marked our strong commitment to reducing the burden breast cancer has on patients and their loved ones. As of 2021, SCOUT surpassed 200,000 procedures worldwide.
As the company expanded, we were able to show our appreciation for employees by offering more services that prioritized their health and wellness. This year Merit Salt Lake introduced the Merit Care Clinic, an on-site practice that provides low-cost healthcare to employees and their dependents. We also opened the Merit Employee Garden, a 1-acre parcel of land that offers fresh produce as well as the opportunity for our team to spend time outdoors.
2017
We were proud to welcome Singapore to our Merit family in 2017 as one of our chief centers for innovating and manufacturing. Our Singapore team has more than 30 years of experience in Critical Care product development; and with its R&D laboratory capabilities, it closely collaborates with government agencies and research institutes.
2022
Today, Merit is a billion-dollar company that continues to have a positive impact on patient lives worldwide. Our family of 6,800 employees make this possible by fulfilling the Merit mission to Understand, Innovate, and Deliver.

To our dedicated team, thank you for your efforts in building the next great healthcare company. We look forward to many more years of making a difference.
Breast Cancer Awareness Month 2022

Merit Medical is committed to reducing the burden that cancer places on patients and their loved ones. During Breast Cancer Awareness Month, we are proud to partner with and support Living Beyond Breast Cancer, a non-profit organization whose mission is to connect people with trusted breast cancer information and a community of support. The LBBC fund specializes in providing underserved communities direct access to care via financial assistant grants.
We are excited to be the first and only surgical oncology company to partner with Living Beyond Breast Cancer. Our partnership with this organization will directly help underserved communities across the nation get the financial help and resources they need to navigate through this difficult time.

— Jean Sachs, CEO, Living Beyond Breast Cancer
SCOUT® Reaches a New Milestone During
Breast Cancer Awareness Month

With more than 350,000 women experiencing wire-free localization with SCOUT, Merit’s promise remains the same—to consistently invest in improving technologies and innovating new platforms that meet patient and physician needs. See how SCOUT is improving the lives of patients all around the world.
Merit Medical Employee Support
The Merit team will also be honoring Breast Cancer Awareness Month worldwide during October.
Check back throughout the month of October and see how employees are contributing to this important cause!

The Aliso Viejo team celebrated BCAM with the annual luncheon, pink Merit shirts and pink smoothies this year. 😊

Our Merit team from Bogotá, Colombia, recently launched SCOUT Radar Localization and is very excited to offer this incredible product to Colombian patients.


At Merit, it’s all about family. Yuma Medina, Merit Technician III, and mom, Osleida Ferrer Rojas, Merit Operator II, show their support for #BCAM by wearing pink together! Thank you for the positivity you bring to our team!
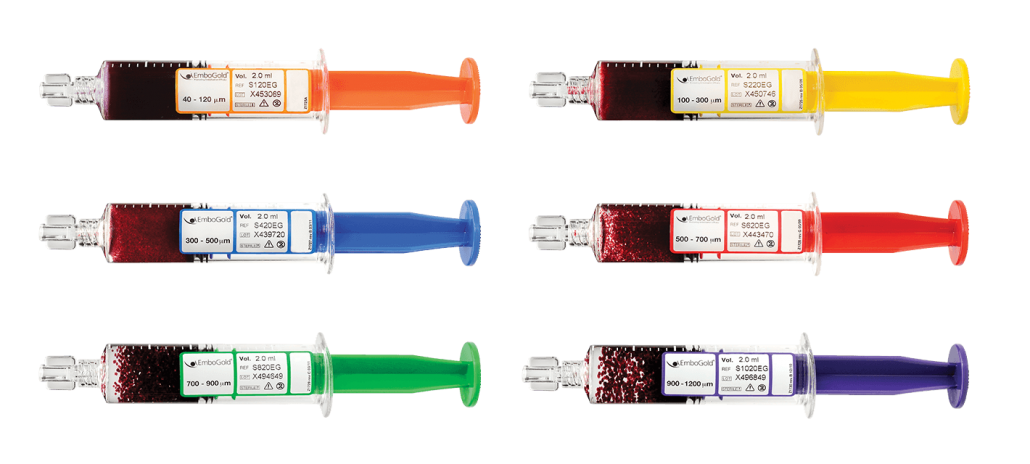
In honor of #BreastCancerAwarenessMonth, our Merit Brazil team coordinated a Pink Out day! We love seeing our global family reflect our commitment to raise awareness and empower people with breast cancer. Nice job, Brazil!

Our Merit Salt Lake Weekend Cleanroom Team is “thinking pink” in recognition of #BreastCancerAwarenessMonth! Thank you to Carina Gonzalez, Cleanroom Supervisor I, for rallying the team!


Meet Rebeca Mortimer, a Merit employee and #BreastCancerSurvivor. By coaching fellow fighters with optimism and compassion, she’s committed to spreading her story to raise awareness of this disease. You’re an inspiration, Rebeca! 💪


Merit Richmond is recognizing #BreastCancerAwarenessMonth, wearing pink as a team to raise awareness and honor those we’ve lost to breast cancer and survivors still with us. A reminder that when we come together, anything is possible.
#WeCare #TeamMerit





It’s #breastcancerawarenessmonth💕
In recognition of Breast Cancer Awareness Month, Merit Galway have donned their pink attire in support of those affected by breast cancer.
The #mariekeatingfoundation was on site and a GP lead cancer awareness seminar were available to all who wished to avail.
A cake sale was organised by our Sports and Social Committee today and tomorrow, to help raise money which will go towards life-changing research and support the amazing work carried out by, National Breast Cancer Research Institute, University Galway.
It’s days like today, we are reminded how kind our employees are!
To all the bakers who made yummy treats for the cake sale and to those who volunteered and donated so generously, Thank You!
Well done team!! 👏 #WearItPink #BreastCancerAwareness #MeritGalway #Support #BCAM22 #WeCare


Merit Asia celebrated Breast Cancer Awareness Month with a variety of #PinkActivities for people of all fitness levels. We dressed up in PINK for #PinkWalk, #HIIT, and even #Picnic!🚶🏻♀️
Whichever we choose, physical exercise and activity are advantageous in reducing the risk of breast cancer. Merit is committed to reducing the burden that cancer places on patients and their loved ones. ❤️ 💪🏻 These are meaningful activities for a worthy cause! #TeamMerit #WeCare #BreastCancer #BreastCancerAwarenessMonth




Closing this Pink October with a great team ! In recognition of #breastcancerawarnessmonth, we would like to thanks everyone for your support in your daily work by providing devices which improve patient quality of life. #Paris #PinkOctober #2022

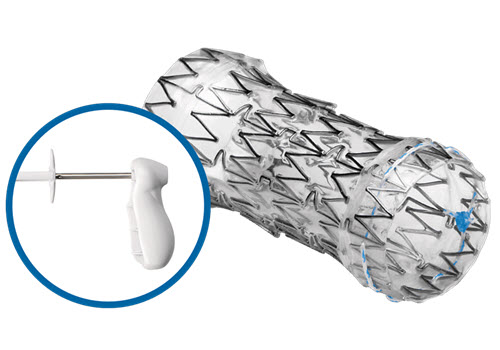
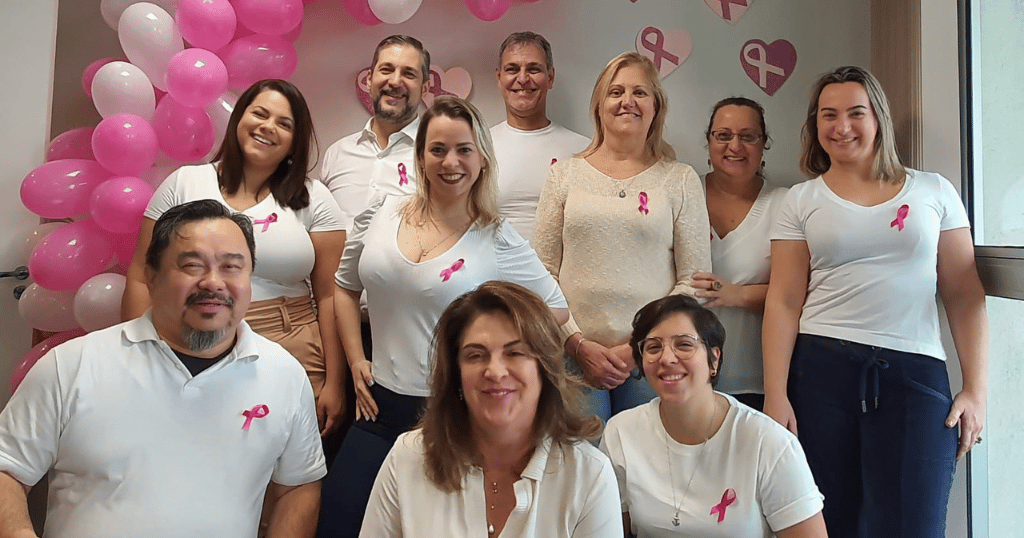
Merit Medical Soft Tissue Biopsy Solutions: Retrieving Samples with Confidence

To help clinicians like you perform biopsy procedures accurately, safely, and with confidence, we offer a wide range of advanced soft tissue biopsy products. From the recently launched TEMNO Elite™ Biopsy System to high-quality legacy products, browse to find the products that best meet your clinical needs:
TEMNO Elite ™ Biopsy System
The new TEMNO Elite Biopsy System is designed to provide you with superior soft tissue samples and total control during procedures. Its advanced features allow for samples 72% larger than competitor side-notch, semi-automatic devices.1 Available in a variety of sizes, the TEMNO Elite is ideal for procedures in many parts of the body, including kidney, liver, and lung.
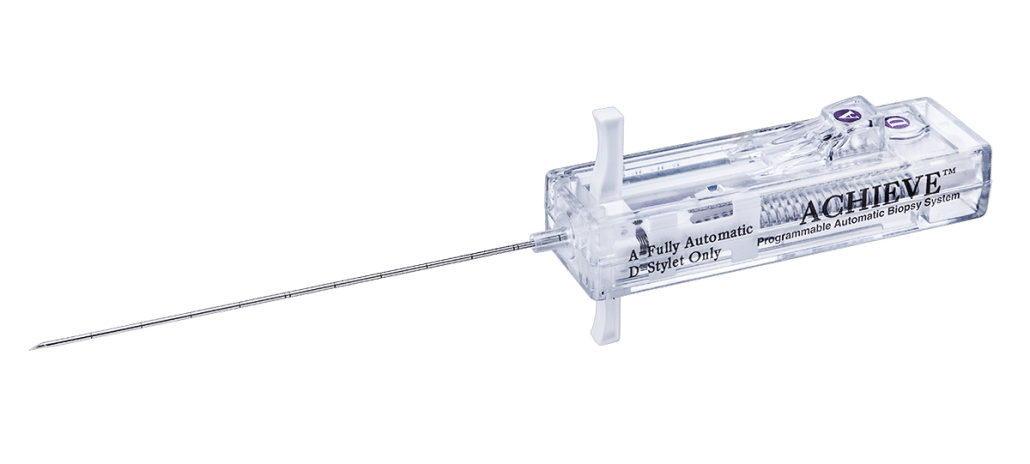
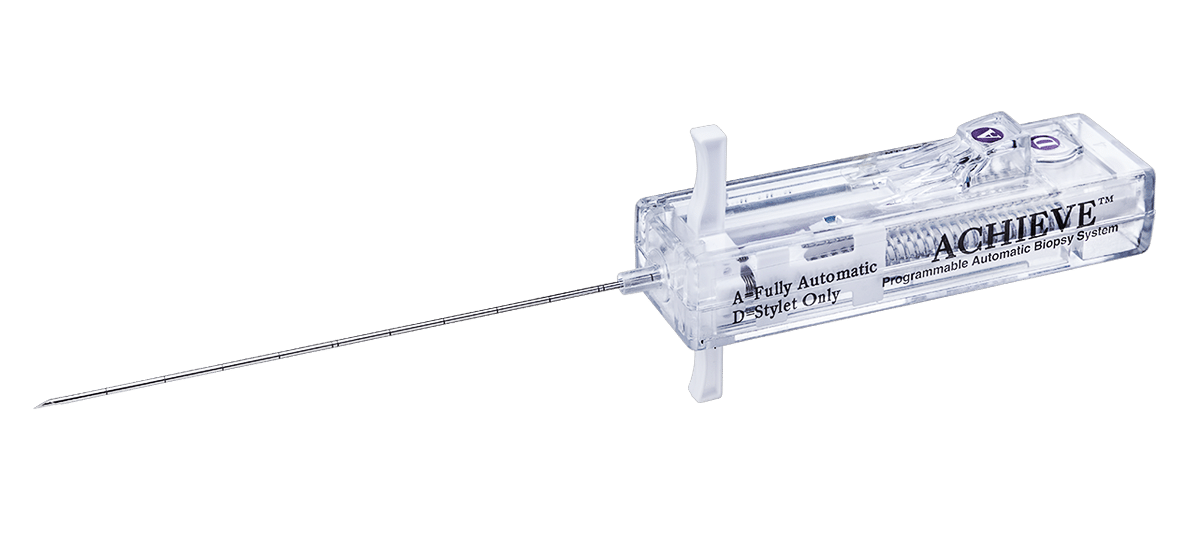
Achieve® Programmable Automatic Biopsy System
With just one hand, you can now benefit from the precise control and quality sampling capability of the Achieve Programmable Automatic Biopsy System. This lightweight, automatic device is spring-loaded for fast, accurate penetration when working with calcified or fibrous lesions. For more precision, the Achieve offers three programmable firing modes.
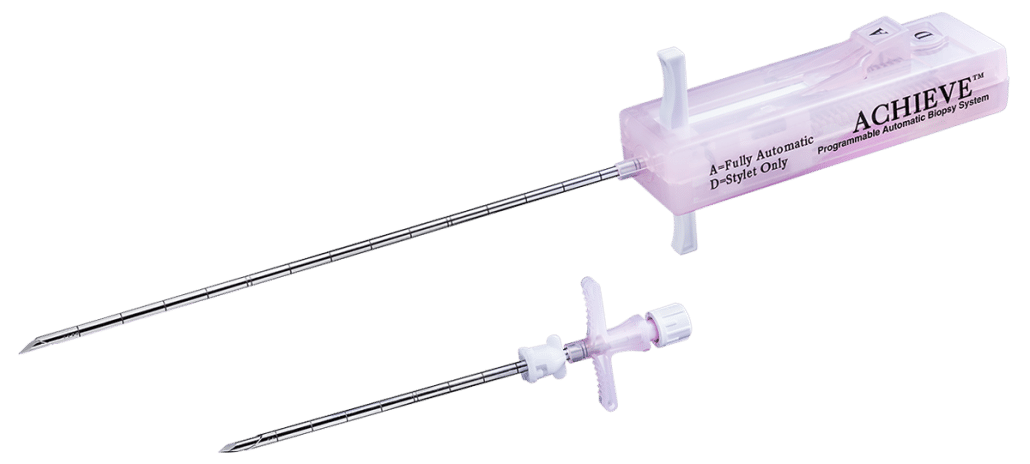
Pink Achieve™ Biopsy Device
The easy-to-use, lightweight design of the Pink Achieve Biopsy Device allows you one-handed use and convenient ultrasound transducer manipulation during breast biopsies. Visualize needle placement before sample retrieval by using the delayed firing option. A coaxial introducer enables multiple sampling from one percutaneous puncture, minimizing damage to surrounding tissue.
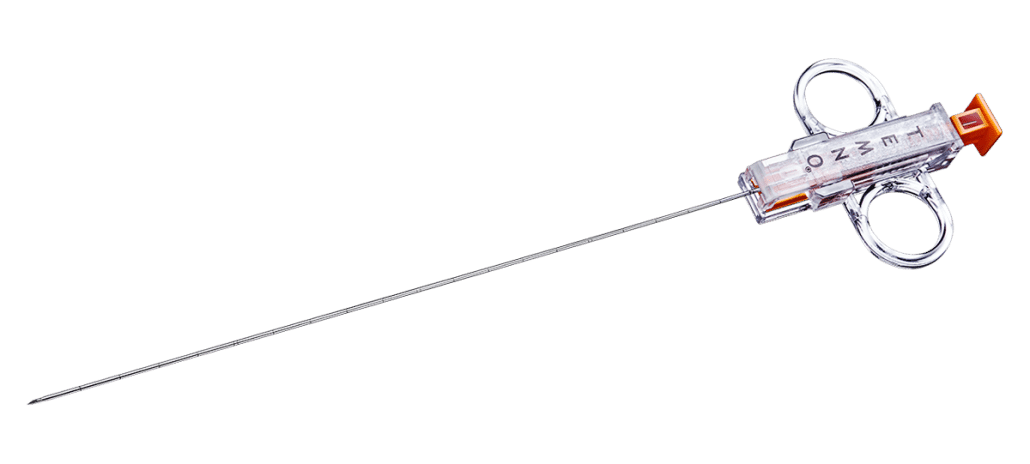
Adjustable Coaxial TEMNO™ (ACT) Biopsy Device
The ACT Biopsy Device allows you to adjust sample size for precise control when working with small lesions and in vascular areas. Reposition the stylet prior to sample capture for greater confidence. Echogenic markings facilitate precise ultrasound placement.
Original TEMNO™ Biopsy Device
Our Original TEMNO Biopsy Device features a 20-mm sample notch for quality sample retrieval and comes in a variety of sizes and gauges. With a sharp bevel tip and depth marks every centimeter (including echogenic markings), it allows you to complete precise sampling for breast, kidney, liver, lung, and thyroid biopsies.
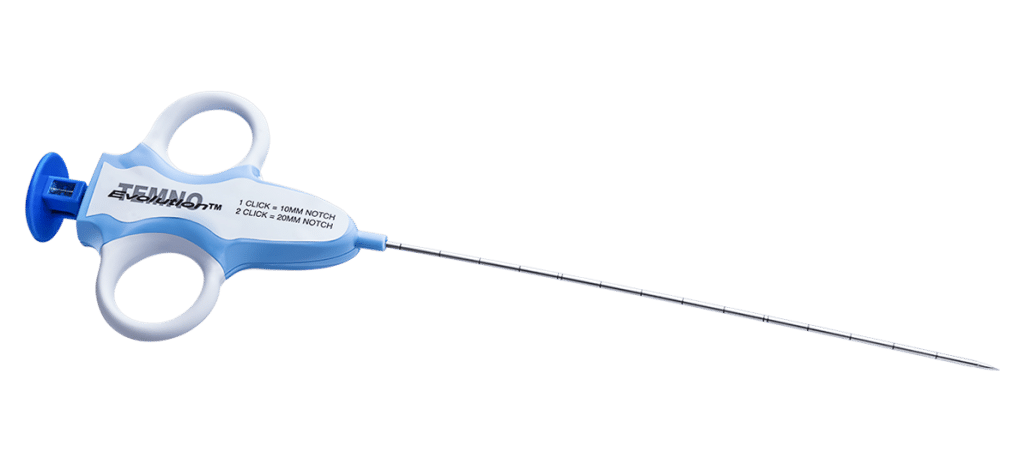
TEMNO Evolution® Biopsy Device
Merit’s TEMNO Evolution Biopsy Device features two notch sizes (10 mm or 20 mm) for clinical flexibility and precise sampling. Its compact, ergonomic design and tactile-enhanced plunger support increased comfort and one-handed operation. The coaxial introducer allows you to collect multiple samples from a single puncture with minimal damage to surrounding tissue.
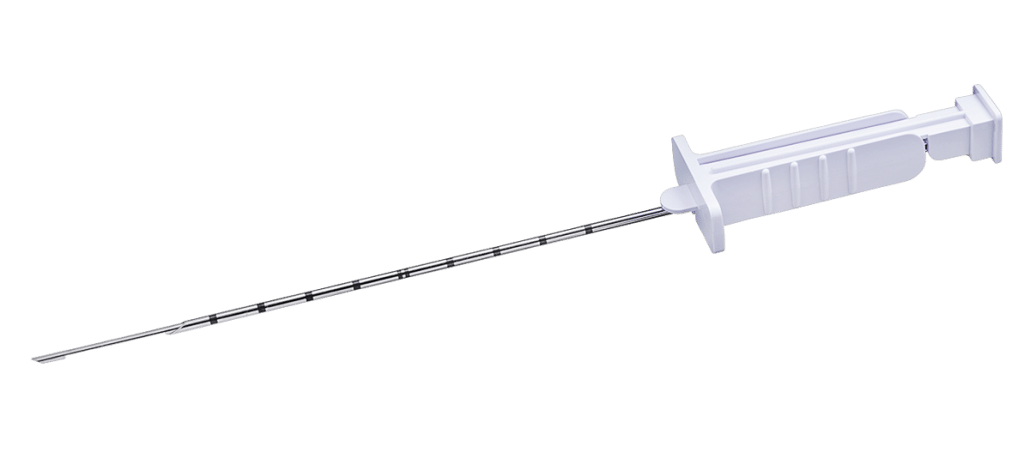
Tru-Cut® Biopsy Device
Manually capture samples with minimal patient trauma using the Tru-Cut Biopsy Device. It features a 20-mm specimen notch, a thin-wall needle to yield a larger core, and removable stylet to obtain multiple tissue samples. Centimeter depth markings assist in needle placement.
At Merit, we’re dedicated to providing high-quality biopsy solutions that help you care for your patients. By working closely with healthcare providers to understand clinical needs, we can innovate new devices and deliver improvements to existing technology to better the patient experience. Talk to your Merit Representative or contact Customer Support to discuss how you can incorporate Merit’s biopsy products into your practice today.
REFERENCES
- Internal testing with 18G. Data on File. Marketing Claims for the TEMNO Elite Device (ECN147270).
- 18 Gauge, Data on file, Merit Medical, 2015.
What’s Your Clinical Challenge? We Have a Solution.
As a leader in customer-focused healthcare, Merit Medical’s priority is to ensure that you have the tools you need to care for your patients. Ranging from product kits to education opportunities, our Complete Solutions simplify preparation and streamline procedures to support quality patient care with a trusted, innovative range of medical devices.
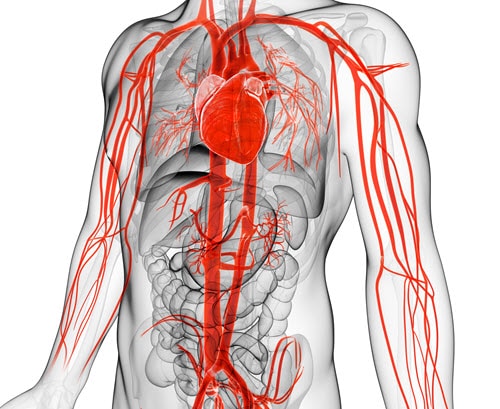
CARDIAC CATHETERIZATION
Our cardiac catheterization solutions provide you with a variety of tools to help you accurately diagnose and successfully treat patients with heart problems. From sheath introducers, like our Prelude IDeal™, and guide wires to catheters, inflation devices, and more, we offer a number of superior devices for your procedures.
CRITICAL CARE
When treating vulnerable patients, every product you use matters. We offer a broad spectrum of tools designed for patients being treated in the critical care unit. Merit critical care technologies aim to reduce contaminant exposure, accurately monitor patient blood pressure, and decrease workplace injury, helping you provide treatment that is safe, effective, and efficient.
DIALYSIS ACCESS
Kidney disease is a global issue, and access is the foundation for any successful dialysis procedure. Our comprehensive dialysis access portfolio, including our catheter-dependence reducing HeRO® Graft, brings reliable and innovative solutions to your practice.
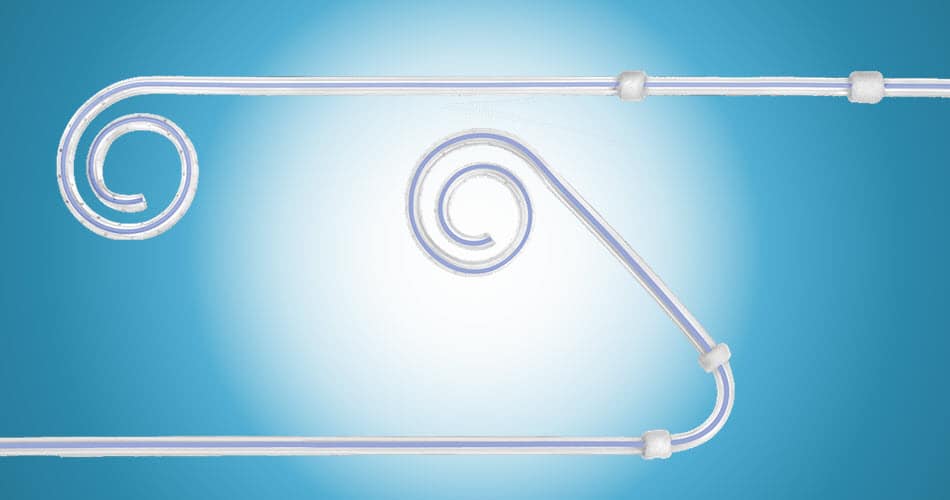
PERITONEAL DIALYSIS
Our home dialysis options offer several patient advantages over in-center dialysis, including better kidney disease-related quality of life. We offer virtual and hands-on physician training, a wide range of catheter sizes, accessories, kits, and patient resources.
RADIAL
Radial access has many well-documented benefits that include improved patient safety, a significant reduction in cost of care, and increased patient and staff satisfaction. We support radial access with a diverse portfolio of innovative products and a world-renowned hands-on physician education program, helping you offer the advantages of radial to your patients.
DISTAL RADIAL ACCESS
Distal radial artery access offers both patient and operator advantages. To help bring these benefits to your practice, we provide advanced training on the distal technique as well as innovative products to support your procedures, such as the first-to-market PreludeSYNC DISTAL™ Radial Compression Device.
DRAINAGE
Over the past two decades, we have continually expanded our drainage portfolio to include a diverse range of solutions that work together to help you achieve optimal drainage care. We offer multiple drainage catheters designed to lessen trauma and promote a more accurate placement.
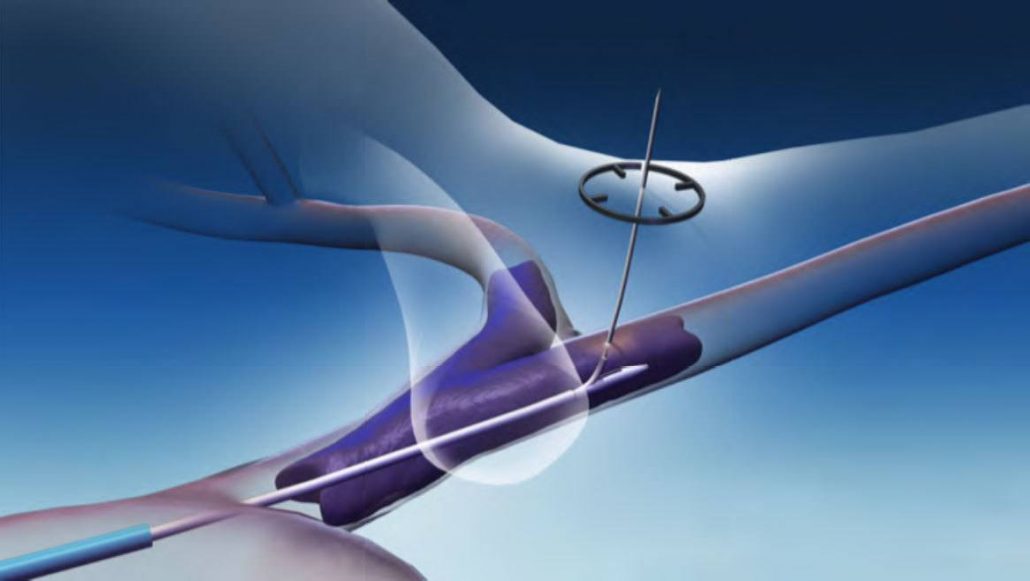
ELECTROPHYSIOLOGY & CRM
Successful diagnosis and treatment of electrical cardiac activity is crucial—this is why we offer a range of physician education courses and specialized tools to assist in making accurate diagnoses and create effective treatment plans. Features include extra-stiff transseptal needles, ergonomic handles for exceptional control, and advanced introducer systems.
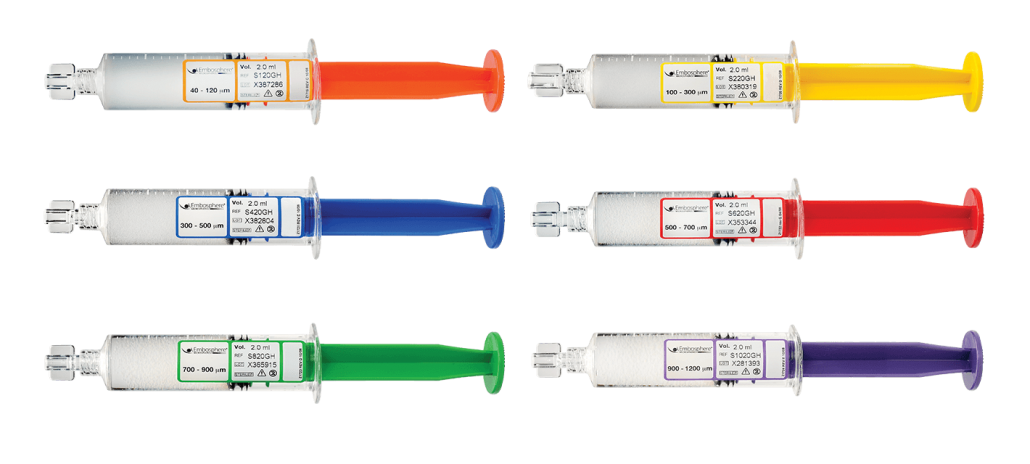
EMBOLOTHERAPY
Our proprietary embolic products are the most studied on the market and allow for efficient and safe delivery and predictable outcomes. To complement our offerings, we provide excellent ongoing customer service to ensure you have the tools you need for your procedures.
To help support your prostatic artery embolization (PAE) practice, we offer virtual and hands-on training, trusted products, clinical resources, patient materials, and more.

Our uterine fibroid embolization (UFE) solutions offer trusted products that deliver predictable clinical results as well as long-term symptom control.
We also offer extensive patient resources at our Ask4PAE and Ask4UFE sites.
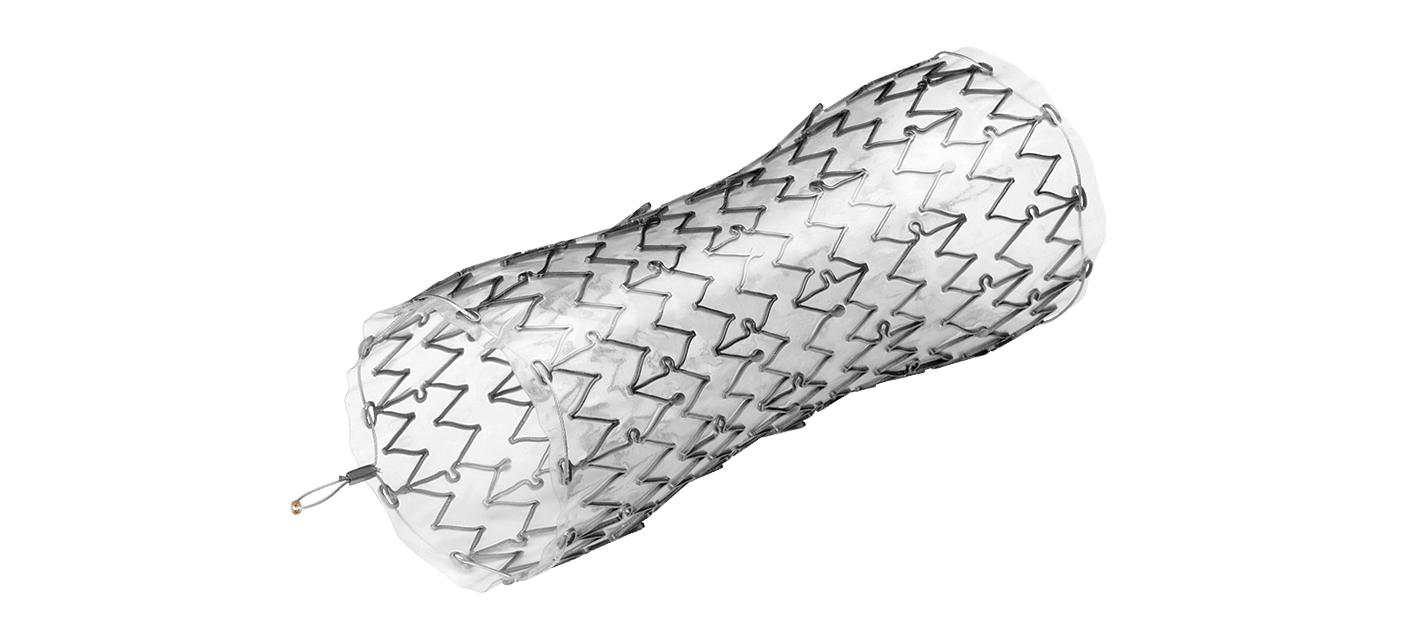
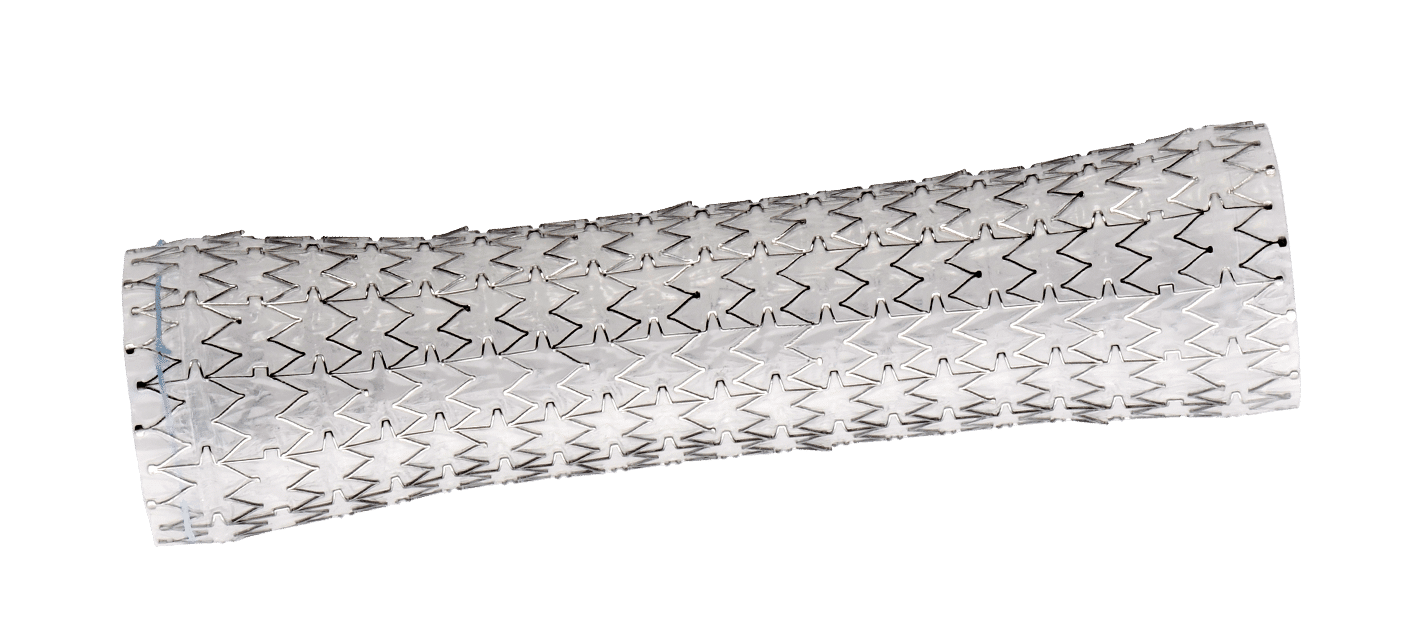
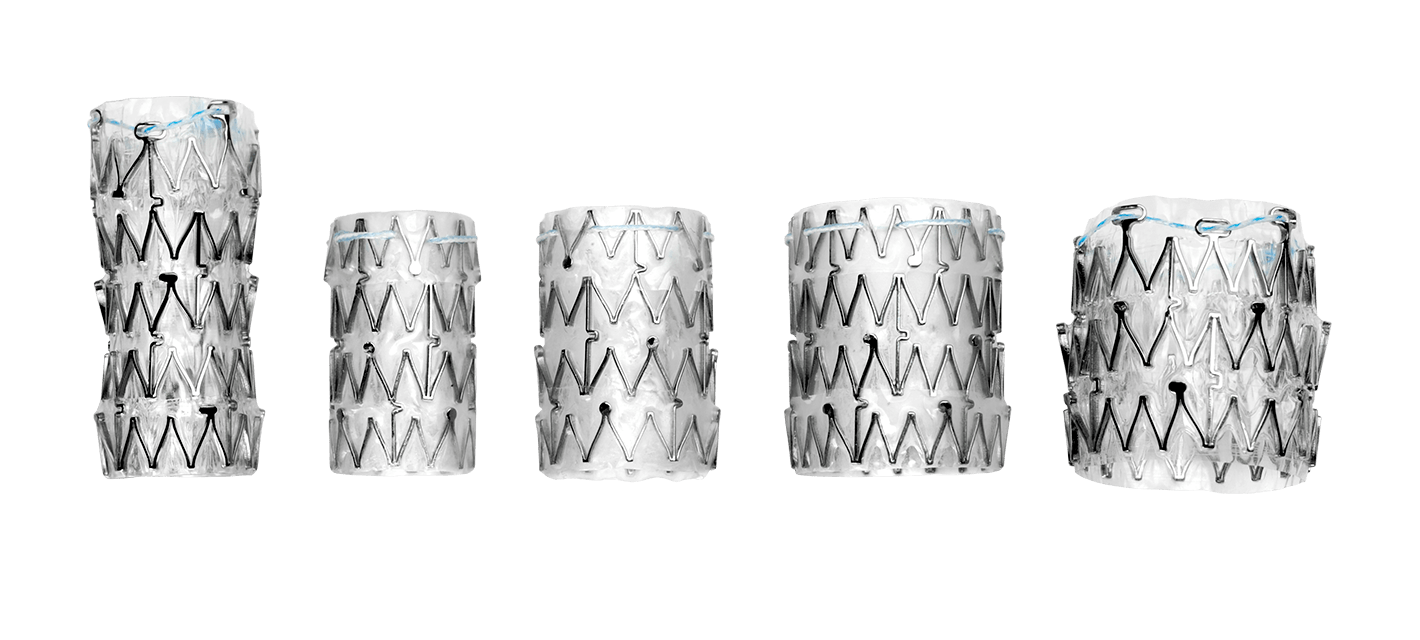
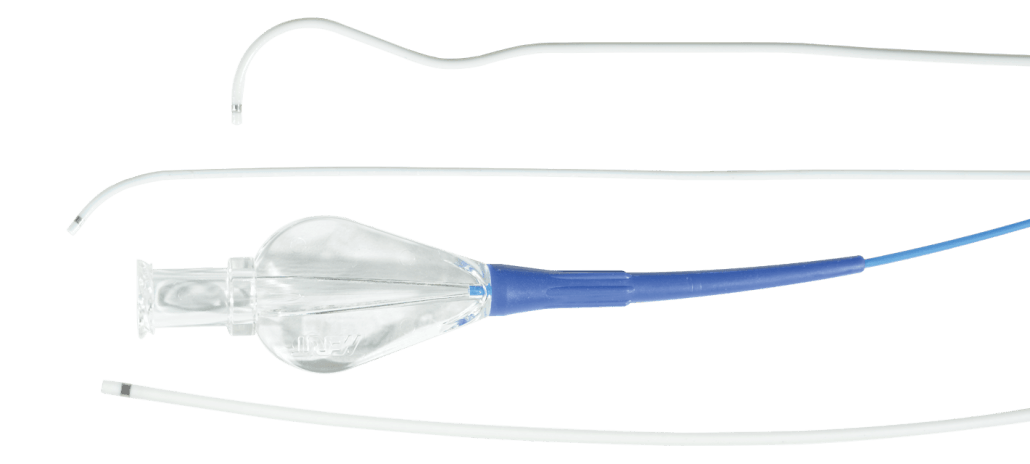
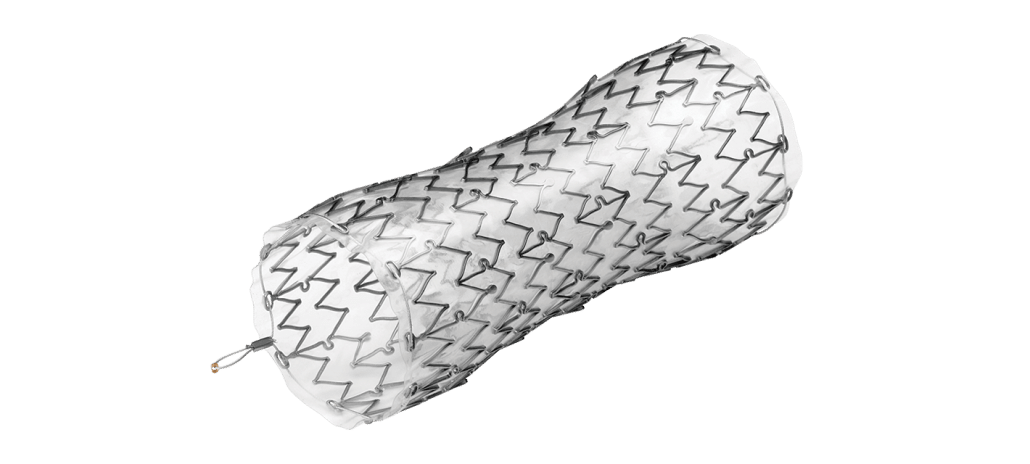
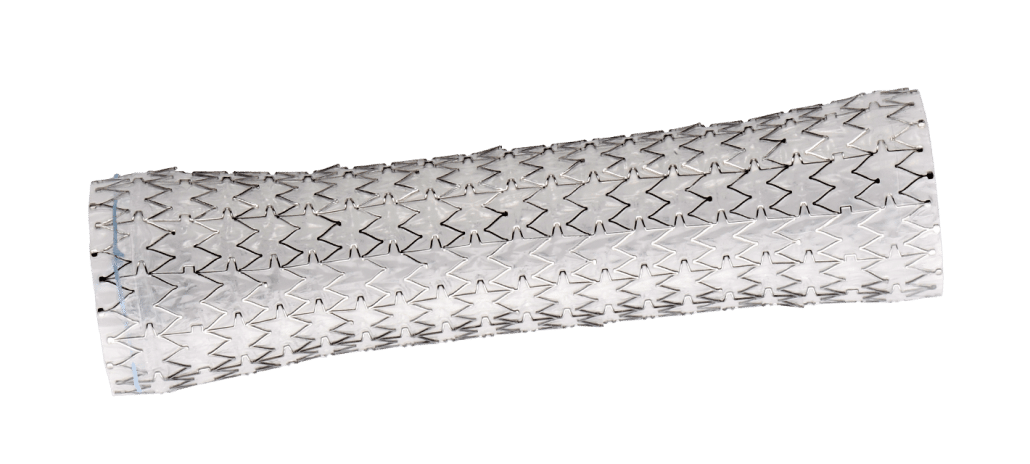
GASTROENTEROLOGY STRICTURE MANAGEMENT
Merit Endoscopy’s fully covered, laser-cut esophageal stent technology provides for accurate placement and minimized migration. In addition to our state-of-the-art stent technology, we deliver best-in-class dilation products, including our BIG60® Inflation Device and our Elation dilation balloons as well as enhanced physician training.
PULMONARY STRICTURE MANAGEMENT
For patients with tracheobronchial strictures, stent technology can provide rapid palliation and improve quality of life. We offer fully covered, laser-cut tracheobronchial stents and advanced over-the-wire and direct visualization delivery systems. Download case studies and participate in virtual and hands-on training—all designed to help you advance patient care.
KITS & PACKS
Designed to bring convenience and efficiency to your office, our kits and packs solutions can help simplify prep and procedure, support quality patient care, and reduce inventory levels. Our team analyzed hundreds of kits and created a set of standard configurations that meet the needs of the majority of cath labs, interventional radiology, and vascular surgery departments. We also offer customizable kits to fit your unique procedural needs.
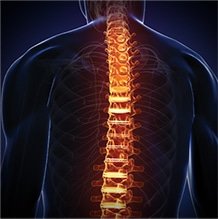
SPINE
Through a diverse portfolio of sophisticated steerable technologies, we deliver complete procedural solutions designed to treat pathologies of the vertebrae, reduce pain, and improve patient quality of life. Our comprehensive education programs and unique products allow physicians to address patient-specific needs and physician preference in the treatment of vertebral pathologies.
VENOUS
Our minimally invasive venous solutions are designed to treat symptoms, minimize post-operative pain, and provide faster recovery. Explore products, accessories, and kits, packs, and trays—each complementing the next to provide you with better patient outcomes.
Merit’s dedication to comprehensive customer care starts with providing the tools you need to treat your patients. Ready to get started? Available via email, phone, and live chat, our Customer Support team is here to help find a solution for you. Browse our virtual in-service and product support videos, all designed to help you obtain additional product knowledge and insights. We look forward to working with you.
Let’s Talk Lung Cancer: An In-Depth Interview with Dr. Reddy

Lung cancer is the leading cause of cancer deaths worldwide.1 In the United States, more people die from lung cancer than any other type of cancer.2 November is Lung Cancer Awareness Month, and to help us gain a better understanding of the condition, the screening process, and treatment options, we sat down with Chakravarthy Reddy, MD, pulmonologist at the University of Utah Huntsman Cancer Institute in Salt Lake City, UT.
What Is Lung Cancer?
Lung cancer occurs when cells in the lungs change or mutate, resulting in abnormal cell growth. These cells multiply uncontrollably, forming a tumor and spreading to other parts of the body.
“Stage one or stage two, where patients are potentially curable, have almost no symptoms at all; it’s always incidentally found,” Dr. Reddy explains. “A patient has a scan for some other reason, and the cancer is detected in the lungs.”
When lung cancer symptoms do manifest, they can include a cough that worsens or does not resolve, chest pain, shortness of breath, coughing up blood, wheezing, weakness or fatigue, and weight loss.4 “Unfortunately, by the time a patient presents with symptoms, they’re in advanced stages, and their survival is not as good,” says Dr. Reddy.
What Are Risk Factors for Lung Cancer?
Smoking is by far the leading cause of lung cancer, putting people who smoke at a significantly higher risk of developing lung cancer compared to non-smokers.5
In addition to smoking, breathing secondhand smoke is also dangerous, increasing the risk of lung cancer.6 “We always talk about smokers, but there is a correlation between people who live with smokers and their risk for developing lung cancer,” Dr. Reddy adds. “Secondhand exposure does increase the risk of developing cancer.”
The American Cancer Society lists other risk factors for lung cancer, which include:5
Radon
A naturally occurring radioactive gas, radon is the breakdown of uranium in soil and rocks. Potential risk areas are homes with basements.
Asbestos
Asbestos is a mineral fiber that occurs in rock and soil.7 People who work with asbestos (e.g., in mines, mills, textile plants, shipyards, and where insulation is used) are several times more likely to die of lung cancer.
Carcinogens
Exposure to cancer-causing agents, such as uranium, arsenic, beryllium, cadmium, nickel compounds, coal products, and diesel exhaust can increase lung cancer risk.
Personal or Family History
If an individual has lung cancer, there is a higher risk of developing another lung cancer. Brothers, sisters, and children of people who have had lung cancer may have a higher risk.
Previous Radiation Therapy to the Lungs
People who have had radiation therapy to the chest for other cancers are at a higher risk of lung cancer, particularly if they smoke.
Air Pollution
In cities, air pollution can increase the risk of lung cancer, with some research suggesting approximately 5% of all deaths from lung cancer may be due to outdoor air pollution.
Who Should Be Screened for Lung Cancer?
The recommended screening test for lung cancer is a low-dose CT scan.8 According to the United States Preventive Services Task Force, those eligible for screening must meet the three-pronged criteria:9
Age ǀ Adults aged 50-80 years
Smoking History ǀ Individuals with a 20 pack-year smoking history
Tobacco Exposure ǀ Current smokers or those who have quit within the past 15 years
Age is a straightforward benchmark, but calculating a pack-year may seem foreign to most. “Multiply the number of packs of cigarettes you smoke per day by the number of years you’ve smoked. This gives you the value, which we call pack-years,” Dr. Reddy explains. An example would be if a person has smoked a pack of cigarettes for 20 years or two packs for 10 years, each of these instances would calculate a 20 pack-year history.
The third criterion addresses tobacco exposure—but what is the significance of a 15-year time span? “It takes about 15 years for the risk [of lung cancer] to normalize,” Dr. Reddy says. “If it’s been less than 15 years since the patient quit, then the third criterion for lung cancer screening is met.”
This also means if a patient does not meet the criteria, screening will not happen. Dr. Reddy encourages people who are under 50 who have a 20 pack-year history to speak with a physician about any concerns, personal risk factors, and the benefits of being screened.
What Lung Cancer Treatment Options Are Available?
When lung cancer is caught early, there are more curative options. Unfortunately, as Dr. Reddy mentioned, lung cancer is normally caught in late stages. A surgery called a lobectomy, which removes one of the lobes in the lung, is only an option for stage 1 or 2 cancer. “Patients who come in with lung cancer don’t have healthy lungs to begin with,” Dr. Reddy says. “It’s more likely they also have emphysema from smoking, and they probably won’t tolerate removal of even a lobe.”
If a patient’s lung function is borderline, Dr. Reddy suggests another surgical option called a wedge resection, where the lobe is spared, and only the cancer is removed. “It’s not preferred, but if that’s the only option, it’s better than not doing anything,” Dr. Reddy says. “If their lung function is any worse than that, then we clearly cannot do any surgery at all. We have to think of second-line approaches, such as radiation therapy.”
According to Dr. Reddy, lung cancer that spreads first to the lymph nodes in the chest is still potentially curable. However, once it leaves the chest and invades the chest cavity and other parts of the body, such as the adrenal glands, the brain, or bones, it is potentially no longer curable. When this occurs, palliative care is the only option, relieving symptoms and mitigating suffering while optimizing patient quality of life.
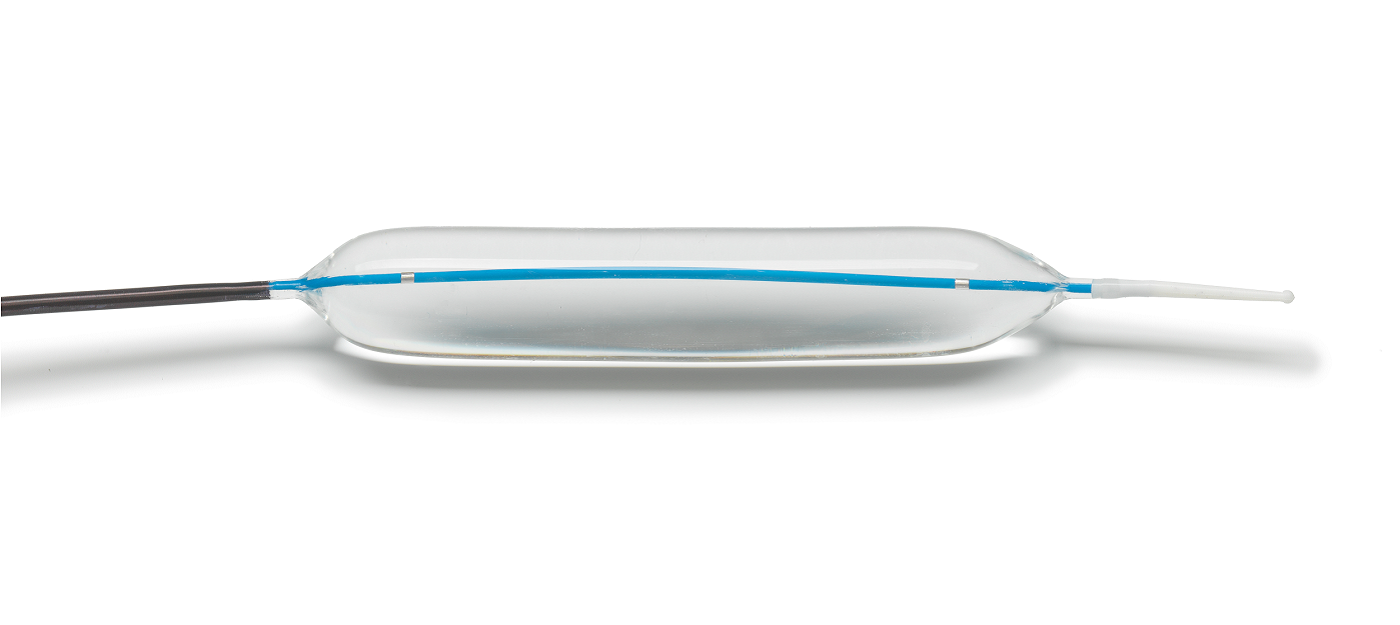
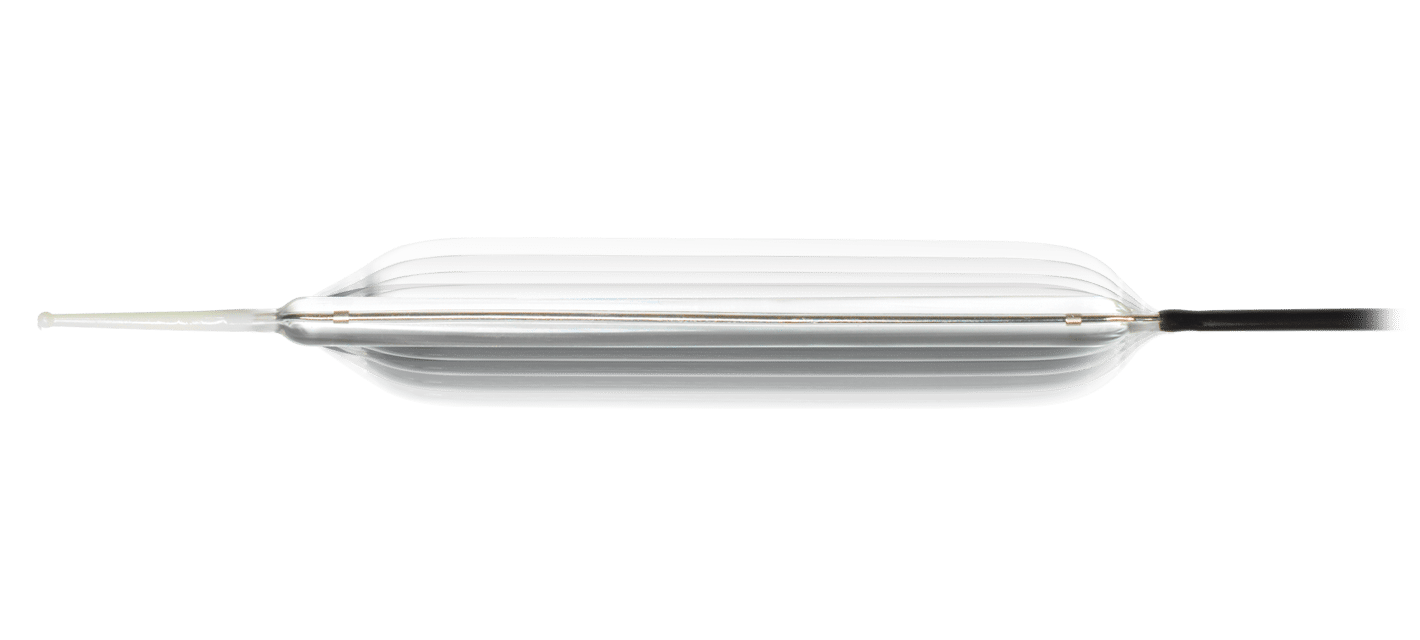
To relieve common lung cancer symptoms, such as shortness of breath or a persistent cough, there are options. “One of the things we do is use balloons to dilate [the airway passages],” Dr. Reddy explains. “Merit makes Elation® balloons, which we find extremely useful, especially because they are available in short, two-centimeter balloon configurations.”
A second approach is to stent the tumor in the lung to maintain the patency of the airway. An option for this line of treatment would be Merit’s AERO® Tracheobronchial Stents. “Patients notice an improvement immediately, almost right after they wake up from the procedure,” Dr. Reddy says. “The radial force of the AERO stent actually keeps the airway open, and that improves shortness of breath.”
Lung Cancer Awareness Resources
As lung cancer awareness is heightened this month, it is critical to share facts about the importance of screening with loved ones and encourage those who smoke to quit.
Knowledge is power, and having health resources to help understand lung cancer better is important. In addition to information about the disease, the below organizations provide a wide range of topics, including survivor stories and ways to get involved throughout the month, helping patients and families in their battle against lung cancer:
Lung Cancer Foundation of America
American Lung Association
GO2 Foundation for Lung Cancer
Support for Merit Employees
If you smoke and need help quitting, sign up for our Employee Smoking Cessation program. Contact Dr. Priest for more information.
Merit Medical is dedicated to improving the lives of people, families, and communities worldwide. Learn more about the trusted interventional and palliative treatment options we offer to help physicians care for lung cancer patients.
References:
- World Health Organization. 2021. “Cancer Key Facts.” https://www.who.int/news-room/fact-sheets/detail/cancer
- Centers for Disease Control and Prevention. 2021. “Lung Cancer Statistics.” https://www.cdc.gov/cancer/lung/statistics/
- American Lung Association. 2021. “Lung Cancer Basics.” https://www.lung.org/lung-health-diseases/lung-disease-lookup/lung-cancer/basics
- Centers for Disease Control and Prevention. 2021. “What Are the Symptoms of Lung Cancer?” https://www.cdc.gov/cancer/lung/basic_info/symptoms.htm
- American Cancer Society. 2019. “Lung Cancer Risk Factors.” https://www.cancer.org/cancer/lung-cancer/causes-risks-prevention/risk-factors.html
- Centers for Disease Control and Prevention. 2021. “Health Effects of Secondhand Smoke.” https://www.cdc.gov/tobacco/data_statistics/fact_sheets/secondhand_smoke/health_effects/index.htm
- United States Environmental Protection Agency. n.d. “Learn About Asbestos.” https://www.epa.gov/asbestos/learn-about-asbestos
- Centers for Disease Control and Prevention. 2021. “Who Should Be Screened for Lung Cancer?” https://www.cdc.gov/cancer/lung/basic_info/screening.htm
- United States Preventive Task Force. 2021. “Lung Cancer: Screening.” https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/lung-cancer-screening
Merit’s Commitment to Breast Cancer Awareness

Throughout October, Merit joins Breastcancer.org to advocate the importance of mammography screening in detecting breast cancer at its earliest stages.
For those diagnosed with breast cancer and undergoing surgery, watch the video below to see how SCOUT® is improving the patient experience.
Want to see how Merit employees were supporting Breast Cancer Awareness in 2021? Take a look here.
A Physician’s Perspective on Wire-Free Localization

INTRODUCTION
Everett Bonner, MD, is a general surgeon specializing in surgical breast oncology at the Baton Rouge Clinic a large, multi-specialty clinic in Baton Rouge, LA. Dr. Bonner joined the group after completing his Surgical Breast Oncology Fellowship at Memorial Sloan-Kettering Cancer Center, New York, NY.
Dr. Bonner performs on average 25-30 breast surgical procedures a month at Baton Rouge General Hospital, which implemented their wire-free program with SCOUT in 2019. Dr. Bonner led the SCOUT implementation and shares his perspectives.
What was your primary motivator in evaluating and switching to a wire-free technology?
I think the biggest motivating factor was the problems we had with wire localization. Let’s be honest, no one likes them, not the physicians and certainly not the patients. Wires were becoming dislodged; patients were a bit “freaked out” about a 10-inch wire hanging out of their breast covered by a paper cup.
I always thought sterilization was an issue. We are always so conscious of this in the OR, yet we have this 10-inch wire that was exposed to all kinds of elements for a few hours. I say that a localization with SCOUT facilitates a more sterile surgery.
I also perform Hidden Scar Surgery, and a wire localization made it very difficult for me to place the incision exactly where I wanted. Utilizing the SCOUT technology has eliminated that issue. I have total freedom to place my incision where the patient will not see it and have a constant reminder of her cancer. In a lot of my cases, I can make one hidden incision under the arm for the tumor and the sentinel node.
It has revolutionized my practice – it has been a game changer.
Were you familiar with other wire-free technologies?

We did not trial SCOUT first. We trialed two other wire-free options, and we were not very happy. With one we had to continuously adjust equipment, and with the other we would have needed to switch to a whole new standard of surgical instruments.
For us, SCOUT was the technology of choice. It was more user friendly, and we would not have to rebuy all new instrumentation. It has worked out extremely well for the hospital, for our practice, and we have never looked back. In fact, my associates and I now almost localize exclusively with SCOUT, and most of us have not used a wire localization in more than a year.
Since using SCOUT, how has it affected your surgical outcomes?
It has been a game changer in three key areas. First and foremost, my re-excision rate is down to less than 5% (the national average is about 10%). I spend less time in the OR, and infection rates have dropped.
I think a very important point is that I use SCOUT, not only for localization, but for real-time guidance during surgery. I am constantly using SCOUT as I am doing my circumferential dissection around the tumor. I am constantly relocating to make sure I am not too close to the tumor, and once I have removed the tumor, I do a margin assessment circumferentially. If it looks like I am too close into a particular margin, I will go back and take additional tissue.
Also, not to be minimized is the fact that I can perform a lumpectomy in about 30 – 45 minutes, as opposed to the hour and a half it normally takes with a wire localization. That is less OR time, less anesthesia for the patient, which all adds up to safety and cost savings.
What can you tell us from a patient’s perspective about a wire-free experience?
Patients love it! I do a lot of patient education upfront, and I am very detailed in explaining the whole surgical experience. I get rave reviews on how “cool” SCOUT, is and they love that they cannot see or feel it, especially patients who have had a past wire localization experience.
At first, I did get a bit of push back about making a trip to the hospital to get the reflector placed, but once I explain that it can be done in conjunction with pre-admission testing, that concern was alleviated.
Patients really appreciate the value of new technology. It is good for them and good for the practice. Being on the forefront of new technology has improved my patient volume. We do little advertising. Therefore, its popularity has been purely by word of mouth.
What are the main outcomes a physician should expect from their wire-free technology?
The number one thing is cleaner margins and the potential to decrease your re-excision rate. Like I mentioned before, my rate is now half of what it was with a wire.
Number two is patient comfort and satisfaction. Patients are nervous enough going to surgery. Add the discomfort and the trauma of a wire sticking out of their breast and that is not patient centric. SCOUT has changed all of that.
The third one, and I think also a major consideration, is precision. You can take less tissue because you know exactly where you are going as you dissect the tumor, which results in a more cosmetically appealing result. Some surgeons say, “Just take a larger tissue sample.” But my question is why when SCOUT is so precise? With this localization and guidance technology, you can take less tissue and have good margins as well as a better cosmetic outcome.
Merit Brings Awareness to Men’s Health During the Month of June

At Merit Medical, it’s our goal to not only provide the tools physicians need to treat and improve patient outcomes but also share knowledge and increase awareness surrounding risk factors for disease.
We understand that illness affects both men and women, but to offer the best patient care, it’s also important to shed light on diseases that are more prevalent in one sex versus the other.
Here are just some of the illnesses that are seen more frequently among men—and how we help care for each.
ESOPHAGEAL CANCER
Esophageal cancer is cancer found in the esophagus—the hollow, muscular tube in your body that carries food and liquid from the throat to the stomach. Men are around three times more likely than women to have esophageal cancer.
- Avoid alcohol.
- Eat more fruits and vegetables.
- Maintain a healthy weight.
- Exercise regularly.
Learn more about esophageal cancer.
MERIT PRODUCTS
LUNG CANCER
Lung cancer is a type of cancer that begins in the lungs. It is the leading cause of cancer deaths worldwide. The overall chance of a man developing lung cancer in his lifetime is approximately 1 in 15, whereas for a woman, the risk is about 1 in 17.
- Quit smoking (or don’t start).
- Stay away from secondhand smoke.
- Test your home for radon.
- Avoid cancer-causing chemicals.
- Live a healthy lifestyle.
MERIT PRODUCTS
KIDNEY FAILURE
Although more women than men are diagnosed with chronic kidney disease, or CKD, men are more likely to reach kidney failure sooner.
Although kidney failure can happen to anyone, men may be more at risk compared to women due to differences in hormones and living unhealthier lifestyles.
- Get a kidney check-up at least every year.
- Control your blood pressure and blood sugar.
- Stop smoking (or don’t start).
- Exercise and eat a healthy diet.
- Maintain a healthy weight.
- If you have an enlarged prostate, talk with your doctor to make sure it’s not blocking your urinary tract.
- Give your doctor a list of any supplements, medicines, and/or hormone treatments you’re taking to ensure they aren’t damaging your kidneys.
Learn more about kidney failure and visit our Dialysis Access Solution page.
MERIT PRODUCTS
AORTIC ANEURYSM
The aorta runs from the heart through the center of the chest and abdomen. It’s the main blood vessel that brings blood to the abdomen, pelvis, and legs. An abdominal aortic aneurysm (AAA) is a life-threatening condition that occurs when the vessel enlarges, putting it at risk of bursting. Men are 4-15 times more likely to develop an AAA than women
- Stop smoking (or don’t start).
- Reduce stress.
- Exercise and eat a heart-healthy diet.
- If you have diabetes or high blood pressure, take the medicines your doctor has prescribed.
Learn more about AAA. To learn more about our packs, wires, and other cardiac products, please visit our Merit Vascular page.
MERIT PRODUCTS
HEART ATTACK
A heart attack, also known as a myocardial infarction, occurs when heart muscle doesn’t receive enough blood. As time passes without receiving treatment, the more damage is done to the heart. The main cause of a heart attack is coronary artery disease (CAD). Researchers have found that throughout life, men are about twice as likely as women to have a heart attack.
- Eat a healthy diet.
- Maintain a healthy weight.
- Exercise regularly.
- Stop smoking (or don’t start).
- Monitor your cholesterol and blood pressure.
- Manage your diabetes.
- Take your prescribed medicines.
Learn more about heart attacks. Explore our Cardiac Portfolio, including our radial sheaths, catheters, wires, and compression devices.
MERIT PRODUCTS
LIVER CANCER
Hepatocellular carcinoma (HCC) is the most common type of primary liver cancer and is most often seen in people with chronic liver diseases, such as cirrhosis caused by hepatitis B or hepatitis C. Worldwide, HCC is the fourth leading cause of cancer death and is 3 times more common among males than females.
- Avoid heavy alcohol use.
- Reduce exposure to aflatoxin B1.
- Stop smoking (or don’t start).
- Get the hepatitis B vaccine.
- If you have hepatitis, work with your care provider to receive treatment.
Learn more about liver cancer. Visit our Hepatic Oncology portfolio.
MERIT PRODUCTS
BENIGN PROSTATIC HYPERPLASIA (BPH)
Benign prostatic hyperplasia, or BPH, is the enlargement of the prostate gland and affects only men. It becomes more common as men get older. Up to 90% of men over the age of 80 have BPH. Although BPH is noncancerous, it can cause bothersome lower urinary tract symptoms.
- Maintain a heart-healthy diet.
- Avoid heavy alcohol use.
- Exercise regularly.
Explore the products we offer to support prostatic artery embolization (PAE), a minimally invasive option to treat BPH.
MERIT PRODUCTS
At Merit Medical, our goal is to improve the lives of people, families, and communities worldwide. An important part of this is caring for men’s health by providing the products and therapies needed for patients to live at their best.
Have questions? Reach out to our Customer Support team.
Before using, refer to Instructions for Use for indications, contraindications, warnings, precautions, and directions for use.
Merit Medical Leads Wire-Free Localization as SCOUT® Procedures Surpass 200,000
Merit Medical has achieved an important milestone as SCOUT surpassed 200,000 procedures—far exceeding any other non-radioactive wire-free device. Launched in 2016, SCOUT has realized remarkable growth and system-wide adoption in the US and global expansion since 2020. Our commitment to ongoing product enhancements, customer training and support, and clinical education contributes to this achievement. However, this milestone would not be possible without the input and support of our valued customers.

HOW DID WE GET HERE? THE SCOUT PLATFORM
With clinically insignificant MRI artifact, there is no restriction on the imaging modalities that can be used effectively throughout a patient’s treatment. This gives physicians the ability to place a reflector at the time of biopsy, prior to neoadjuvant chemotherapy (NAC), and to enable targeted axillary dissection. While SCOUT has been used primarily for breast tumor localization, physicians are recognizing the clinical benefits, including 1+/- mm accuracy, 60-mm depth, and 360° detection, are applicable for myriad oncological applications, including nodes, sarcoma, and lung.
1+/-
mm
Accuracy
60 mm
Depth
360°
Detection
OUR COMMITMENT TO YOU
Merit Medical remains committed to you, your staff, and the patients you serve. We are dedicated to delivering exceptional customer service as well as more product enhancements and platform expansion to help reduce the burden cancer places on your patients and their loved ones. Thank you for your ongoing support and partnership through our journey to market leadership in wire-free localization with SCOUT.
Merit Medical to Exhibit at Virtual ASBrS 2021: Products and Symposia You Won’t Want to Miss

We look forward to connecting with you virtually and encourage you to visit the Merit virtual booth to learn of our latest product platform enhancements and clinical updates.
We are also sponsoring a very compelling industry symposium and two learning sessions, all featuring key opinion leaders and experts in breast cancer care. Mark your calendars to include these products and symposia you won’t want to miss:
PRODUCTS
As a provider of world-class solutions for the diagnosis, localization, and treatment of cancer, Merit Oncology consistently invests in improving technologies and innovating new platforms to meet physicians’ needs.
SCOUT® RADAR LOCALIZATION

Explore clinical data and hear why physicians choose SCOUT.
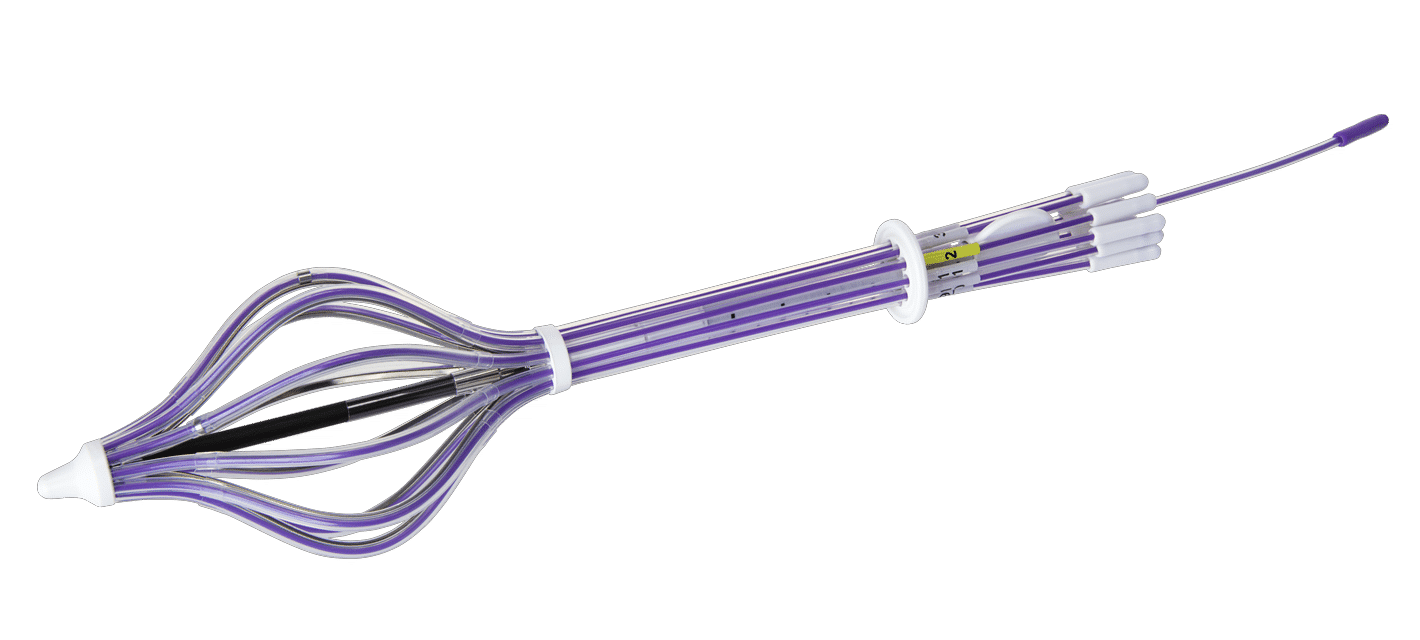
SAVI® BRACHY
ACHIEVE® PROGRAMMABLE AUTOMATIC BIOPSY SYSTEM
SYMPOSIA
ASBrS Breakfast Symposium

The Preferred Localization Solution to Treat More Patients: SCOUT
Friday, April 30, 2021
9:00 am – 10:00 am EDT
Description:
SCOUT Radar Localization exclusively spans the care continuum from time of biopsy placement and targeted axillary dissection to excellent surgical outcomes. Discover the state-of-the art localization techniques practiced by key opinion leaders from Cleveland Clinic, Columbia University, University of Colorado, Intermountain Healthcare, and the Advocate System.
Learning Sessions

The Pathway to Market Leadership and the Future of Radar Localization
Includes physician education recording with Michelle Carpenter, MD
Friday, April 30, 2021
2:45 pm – 3:15 pm EDT
Description:
At the time of the 2021 ASBrS meeting, SCOUT will have achieved an important milestone—200K procedures, far exceeding any other wire-free technology.
Join David Gilstrap, Director of Global Product Management at Merit, to learn more about what differentiates radar localization and what is on the horizon for platform enhancements. His presentation will include a physician education recording with Michele Carpenter, MD.

Start-to-Finish APBI in 2 Days: Three-Fraction Treatment with SAVI
Saturday, May 1, 2021
9:15 am – 9:4 5am EDT
Description:
Interested in learning about three-fraction APBI with SAVI? Listen to UC San Diego’s Cate Yashar, MD, and Dan Scanderbeg, PhD, as they discuss outcomes of the TRIUMPH-T Trial, provide an assessment on patient satisfaction, and discuss adopting a three-fraction TRIUMPH-T protocol in your practice.
At Merit, our goal is to lessen the burden cancer places on patients and their loved ones by offering products and services that make this possible. We look forward to seeing you at virtual ASBrS 2021!
*Before using any of the Merit products mentioned above, refer to Instructions for Use for indications, contraindications, warnings, precautions, and directions for use.
REFERENCES
- Khan AJ et al. 2019. “Three-Fraction Accelerated Partial Breast Irradiation (APBI) Delivered With Brachytherapy Applicators Is Feasible and Safe: First Results From the TRIUMPH-T Trial.” Int J Radiat Oncol Biol Phys 104, no. 1:67– PMID: 30611839.
Helping You Understand Esophageal Cancer

Across the nation, Americans are recognizing April as Esophageal Cancer Awareness Month—a full 30 days dedicated to learning more about the disease, signs and symptoms of it, and steps individuals can take to reduce their risk.
This year alone, it’s estimated there will be more than 19,000 new esophageal cancer cases diagnosed and more than 15,000 deaths from the disease in the United States.
To help this patient population, our goal at Merit Medical is to not only provide the tools physicians need to treat and improve outcomes for individuals with esophageal cancer but also share knowledge and increase awareness surrounding the disease.
Use the following infographics and resources to inform yourself and prepare for a discussion with your doctor about your own personal risk.
WHAT IS ESOPHAGEAL CANCER?

Esophageal cancer is cancer found in the esophagus—the hollow, muscular tube in your body that carries food and liquid from the throat to the stomach.
ESOPHAGEAL CANCER RISK FACTORS
Although a rare condition, esophageal cancer has an average five-year survival rate of approximately 20%.
Risk factors for developing esophageal cancer include the following:




If you’re experiencing heartburn that’s severe or frequent, it’s important you talk with your doctor. The longer it continues, it can damage the inner lining of the esophagus, leading to a condition called Barrett’s esophagus, which increases your risk of esophageal cancer.
Find help to stop smoking and support to reduce alcohol consumption.
Learn more about other risk factors, including how men are three times as likely as women to suffer from esophageal cancer.
MOST COMMON TYPES OF ESOPHAGEAL CANCER
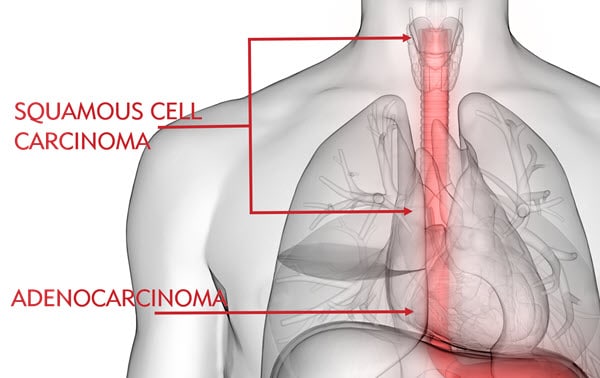
Esophageal cancer is most common in two forms: squamous cell carcinoma and adenocarcinoma. Squamous cell carcinoma typically affects the upper and middle esophagus, whereas adenocarcinoma is commonly found in the lower esophagus near the stomach and is believed to be related to stomach acid exposure. Learn about other forms of esophageal cancer.
Adenocarcinoma is the most common type of esophageal cancer among Caucasian people, whereas squamous cell carcinoma is more common among African Americans. In comparison, American Indian/Alaska Natives, Hispanics, and Asians/Pacific Islanders have lower rates of esophageal cancer, respectively.
SIGNS & SYMPTOMS
Esophageal cancer can be difficult to treat because individuals don’t usually experience symptoms until the disease is advanced. Esophageal cancer usually doesn’t cause symptoms in its early stages.
As it progresses, symptoms can include:
- Difficulty swallowing, can be painful
- Hoarse voice
- Indigestion or heartburn
- Weight loss
- Persistent cough
- Vomiting
Some risk factors for esophageal cancer can’t be avoided, such as genetics or age. However, there are many lifestyle changes that can help you reduce your risk, such as avoiding tobacco and treating acid reflux:

DIAGNOSIS & TREATMENT
If you’ve been diagnosed with esophageal cancer, you most likely have many questions. You also have multiple treatment options. Your cancer care team will discuss each with you, helping you make the best decision for you.
Learn more about esophageal cancer diagnosis, treatment, and life after treatment or visit the Esophageal Cancer Action Network (ECAN) for a free patient guide.
MORE RESOURCES
- American Association for Cancer Research
- American Cancer Society
- Cancer Care
- Cancer Support Community
- Esophageal Cancer Awareness Association
- ECAN
- National Cancer Institute
- National Foundation for Cancer Research
RELATED PRODUCTS
“When You Are Informed, You Hold the Power” – Sharon Huff, SCOUT® Patient
“A close friend and I are going through this breast cancer journey together. She is a few weeks ahead of me in her diagnosis, so I have learned a lot from her experience,” Sharon said. “She had a wire localization and told me, in her words, it was going to freak me out. She had the wire put in very early the morning of her surgery and had to be still, so the wire wouldn’t move. Moving the wire could result in not being able to accurately locate the cancer.”
It came time for Sharon’s surgical consult with Dr. Jonsson at Kaiser Ontario Medical Center, and she was expecting to learn of her surgery date and hear about the wire localization procedure. This weighed heavily on Sharon’s mind. When Dr. Jonsson told her she would be having a wire-free localization, she was pleasantly surprised and relieved.
Although Sharon has an extensive educational background and is an avid reader and researcher, she had never heard of a reflector placement with SCOUT®. She immediately turned to the internet. Sharon read everything she could find about the procedure and watched videos to familiarize herself with what the reflector looked like and how it was placed.
When it was time for her reflector placement with Dr. Nguyen of the radiology department at Kaiser Fontana Medical Center, she was well informed and prepared. “The procedure to implant the reflector was easy and did not take long at all,” Sharon commented. “I was very impressed.”
COVID-19 adds additional stress to any medical procedure. In Sharon’s case, her husband was not allowed to accompany her and instead had to wait in the car. On the day of surgery, she only had to arrive two hours prior to the surgery start time, making her husband’s wait time much shorter than if she would have needed a wire localization on the day of surgery. “Having that little reflector made our day so much smoother and shorter,” Sharon recounted.

When asked to share pearls of wisdom for individuals going through the breast cancer journey, Sharon had three: inform yourself, make your own decisions, and advocate for yourself. “When you are informed, you hold the power,” Sharon said. “And you can feel better about your choices.”
Disclaimer: This information is not intended nor recommended as a substitute for medical advice, diagnosis or treatment. Always seek the advice of a qualified physician regarding any medical questions or conditions.
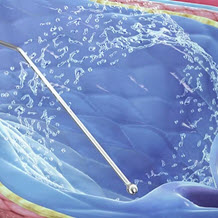
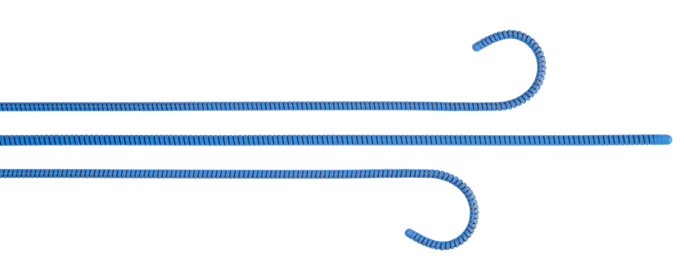
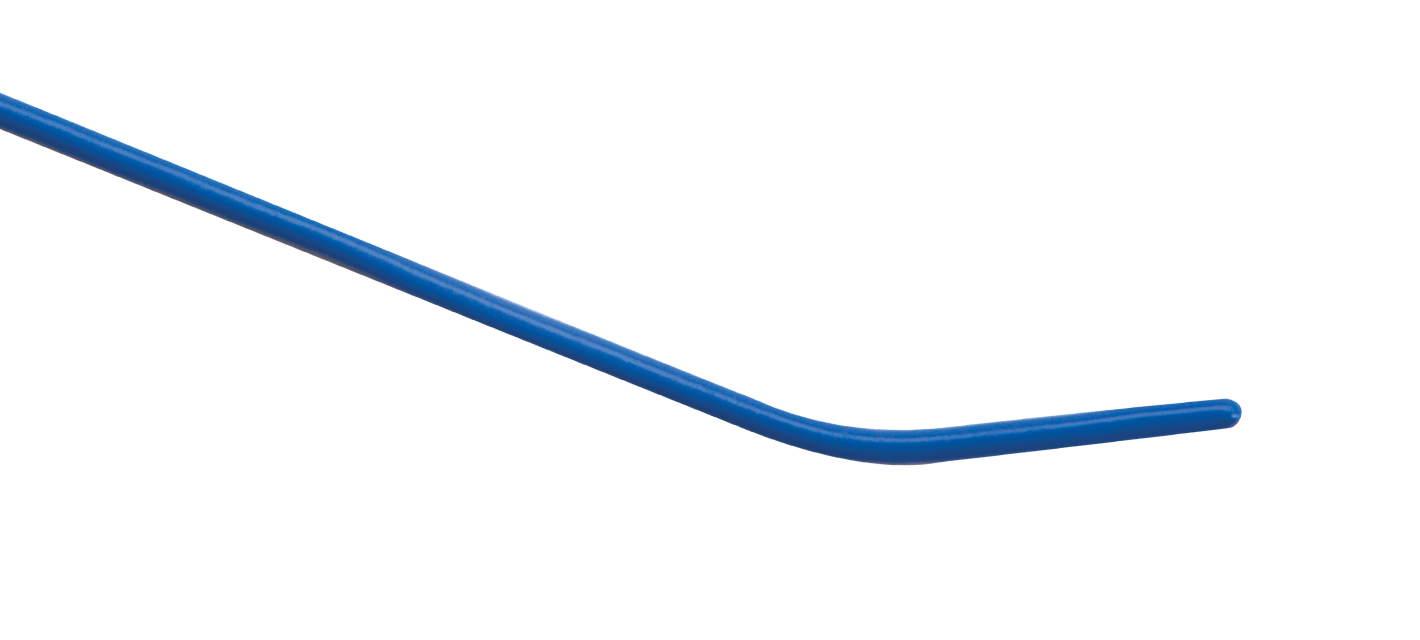
SwiftNINJA® Overcomes Challenges of Selective Catheterization
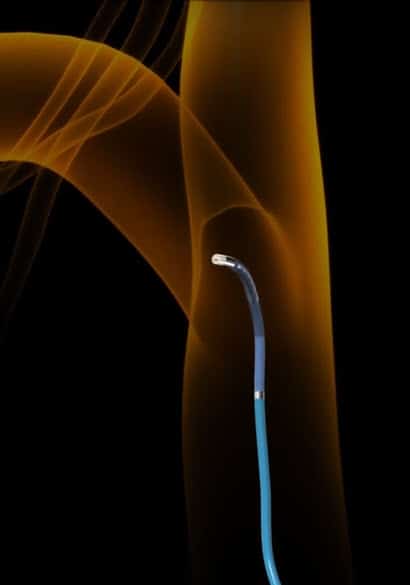
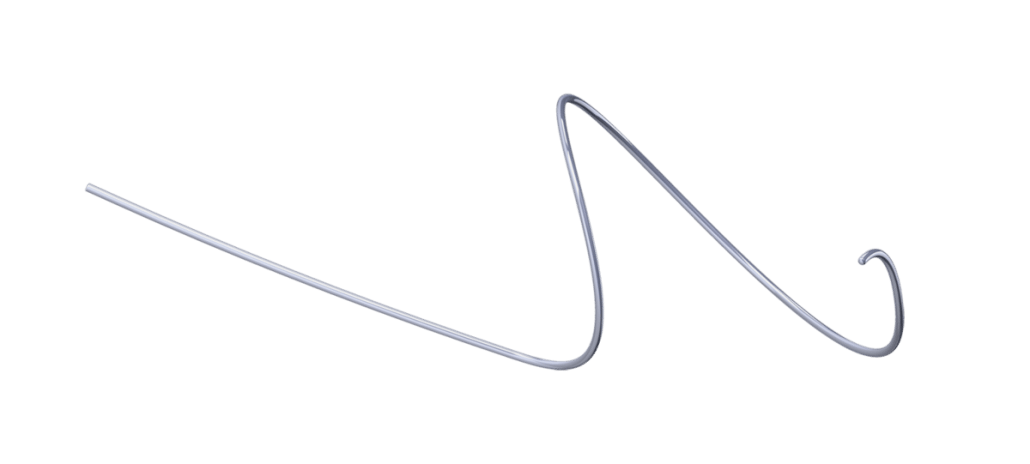
Selective catheterization can be associated with several challenges, such as acute angle branching, blood vessel tortuosity, and small targeted vessel diameter.1 The SwiftNINJA Steerable Microcatheter by Merit Medical, a straight tip catheter that articulates up to 180 degrees in opposing directions, is designed to rapidly select challenging vascular ostium.
A case report by Soyama et al.1 found multiple benefits to using the SwiftNINJA in catheterizations involving acute angle branches as well as a new technique of intentional folding of embolization coils for compact coil packing. The authors found that using a steerable microcatheter made the procedure easier compared to using a conventional device.
The study, published in CardioVascular and Interventional Radiology,1 discussed the following two cases:
CASE 1: CATHETERIZATION OF ACUTE ANGLE BRANCHES
A male patient in his 60s presented with an angiomyolipoma of the left kidney. CT images showed an 8-cm tumor of the left kidney, which had enlarged. To prevent tumor rupture, transcatheter arterial embolization was conducted.
Using the Seldinger technique, a 5F J-shaped sheath introducer was placed percutaneously into the aorta via the left femoral artery. Selective left renal arteriography was performed with a 4F cobra-shaped catheter.
The arteriogram showed two arterial branches of the superior renal capsular artery supplying the primary blood flow to the tumor, both branching out from the main left renal artery with an acute angle of origin. Due to the acute angle branching, Soyama and his team were unable to selectively insert a manually tip-shaped guide wire and instead used the SwiftNINJA as follows:
Bent the tip to turn the orifice of the targeted branch by dial manipulation at the proximal handgrip. Fixed the shape of the tip with the dial stopper.
STEP 2:
Inserted a 0.016-in guide wire into the targeted branch.
STEP 3:
Unlocked the dial stopper. Pushed the microcatheter deep into the targeted branch using the over-the-wire method.
RESULTS:
Catheterization of two targeted branches was completed within 3 minutes. Successful embolization of the target branches followed.
CASE 2: INTENTIONAL FOLDING OF METALLIC COILS IN THE BLOOD VESSEL
A male patient in his 60s presented with right maxillary cancer and was admitted for transcatheter arterial infusion chemotherapy combined with irradiation.
A 5F sheath introducer was percutaneously placed into the aorta via the right femoral artery followed by selective insertion of a 5F catheter into the right common carotid artery. The SwiftNINJA was then inserted into the right internal and external carotid artery.
Selective angiogram showed the targeted tumor was being supplied by the right internal maxillary artery, the transverse facial artery, and the facial artery. It was embolized with pushable metal coils with the intention of creating compact packing of the coils to strengthen the embolic effect and prevent reperfusion:
STEP 1:
Bent the tip of the SwiftNINJA inside the blood vessel using the proximal dial, maintained tip shape, and slowly pushed the coil. The coil was intentionally folded by the change in tip direction. Compact packing was achieved.
STEP 2:
Pushed the second coil into the targeted blood vessel in the same way, completing the embolization using compact coil packing of the right superficial temporal artery.
In procedures such as these, selective catheterization can be very difficult, in some cases forcing a physician to abandon the catheterization all together—even if the shape of the guide wire and catheter was chosen to fit a desired vessel branch.1
In contrast, the SwiftNINJA “has the potential to make selective catheterization easier than when using the conventional device, due to the ability to control the tip shape,” the authors write.1
In the first case,1 the SwiftNINJA allowed the user to shape the tip to the targeted branches easily and properly when needed. It could also be manipulated during catheterization without removing it to reshape the tip, which the authors said could potentially make selective catheterization easier.
The authors1 suggested that in the second case, the SwiftNINJA could be useful for both selective catheterization and compact packing of metallic coils where adjusting and maintaining microcatheter tip shape can be a challenge. Using a steerable microcatheter, they write, “enables the user to easily create an initial loop of the inserted coil and intentionally fold the coils with the stiffly bent catheter tip.”
Soyama et al.1 concluded that the SwiftNINJA “has the potential . . . to allow difficult catheterizations to be completed more easily.”1
SWIFTNINJA KEY FEATURES

Several features and benefits enable the SwiftNINJA to be the solution needed during challenging interventional procedures:180-Degree Steerable Tip The SwiftNINJA’s steerable tip provides speed, navigation, and support—even in the most challenging vascular anatomy. An ergonomic steering dial enables the catheter tip to be deflected from straight to opposing directions up to 180 degrees, allowing for in vivo steering control.
Steering Lock Once the SwiftNINJA’s tip is positioned at a desired location, it can be locked to hold the shape of that position. The tip will remain positioned for embolic placement without the worry of recoil, loss of position, or embolic displacement.
Multi-Dimensional Steering Once the catheter is shaped into a desired position, the SwiftNINJA can then be torqued and advanced through the vasculature, providing 3D steering as it moves in two planes simultaneously.
Tungsten-Braided Shaft Built with a tungsten-braided shaft, the SwiftNINJA provides support and pushability when navigating tortuous vasculature.
Cost Efficiency Because the SwiftNINJA can navigate through complex blood vessels and reach target anatomy quickly, it can be a cost-effective option compared to failed attempts using numerous catheters. As mentioned by Soyama et al.,1 the SwiftNINJA made their procedure easier to perform than using a conventional device.
Similarly, another case study by Hinrichs et al.2 described successful coil embolization of a small hepatointestinal collateral with the SwiftNINJA after failed attempts with other catheters. Henrichs et al.2 write, “taking into account the numerous regular microcatheters that were used without success in our two cases, the appropriate use of a steerable microcatheter can be even more cost-effective with regard to the total material costs.” Merit Medical is committed to providing the medical devices needed to improve and transform healthcare. Discover the SwiftNINJA Steerable Microcatheter by visiting the product page and the Merit Medical Customer Support Center for more information.
RELATED PRODUCTS
References
1. Soyama et al. 2017. “The Steerable Microcatheter: A New Device for Selective Catheterization,” CardioVascular and Interventional Radiology 40, no. 6: 947-952, PMID: 28138724.
2. Hinrichs et al. 2017. “Coil Embolization of Reversed-Curve Hepatointestinal Collaterals in Radioembolization: Potential Solutions for a Challenging Task,” Radiology Case Reports 12, no. 3: 529-533, PMID: 28828119.
Arcadia™ Steerable Technology Provides Unique Benefits to Vertebral Augmentation Treatment
Vertebral compression fractures (VCFs) are the most common fracture in patients with osteoporosis.1 Although painful and debilitating, VCFs often go untreated. To help care for this patient population, Merit Medical innovated the Arcadia, an intuitive balloon-assisted vertebral augmentation (kyphoplasty) system. Designed to be used with the steerable PowerCURVE® Navigating Osteotome, the Arcadia offers several unique benefits when treating patients with painful VCFs.
Bipedicular Footprint, Unipedicular Approach
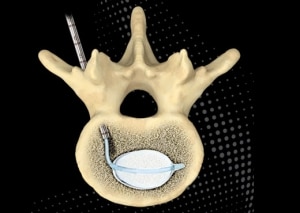
Steerability allows the Arcadia system to target a specific location within the vertebra using a transpedicular approach through a single skin incision. Once past the pedicle body junction, the ability to articulate the device allows accurate navigation to the biomechanically critical important anterior and middle third of the vertebra, resulting in a bipedicular cement footprint byway of a less invasive unipedicular approach.
Unipedicular access has other clinical advantages as well. A systematic review and meta-analysis published in Pain Physician2 compared the safety and efficacy of unipedicular and bipedicular vertebral augmentation approaches in the treatment of osteoporotic VCFs. Results showed that the unipedicular approach required less procedural time, lower radiation dose, and a reduced cement leakage ratio with similar clinical outcomes in pain relief, decreased disability, and improved short and long-term general health.
Reduced Procedural Radiation Exposure
The use of fluoroscopic guidance in the transpedicular treatment of VCFs is necessary for visualization; however, radiation exposure must be limited when possible. The single access unipedicular approach, as provided with the steerable Arcadia, has the potential to reduce radiation exposure.2 Radiation exposure to patients undergoing unilateral vertebral augmentation has been shown to be 50% of the dose received by patients who receive bilateral treatment.2
Safe Transpedicular Access

Transpedicular steerable access, as made possible with the Arcadia and the PowerCURVE, is intended to enable safe passage past the pedicle body junction into the vertebral body. This approach offers advantages, including avoidance of the radicular spinal arteries, which are vulnerable when using an extrapedicular approach. This is significant given spinal arteries, such as the artery of Adamkiewicz, usually arise from the level of the ninth intercostal artery to the second lumbar artery.3
Further, Liu et al. reported that extrapedicular vertebral augmentation in the lumbar vertebrae had a risk of injuring the lumbar artery and was not recommended for use in L4 and L5, especially in female patients.4 Given this data and the size of lumbar vertebrae, transpedicular access with the steerable Arcadia and PowerCURVE devices may be an appropriate treatment option for this patient population.
Transpedicular access through the pedicle using steerable devices also reduces the oblique angle required when using rigid straight devices, decreasing the risk of breaching the medial cortex and cement leakage within the spinal canal.5
Enhanced Navigation
Compared to curved devices manufactured with a predetermined shape which limits trajectory based solely on access into the vertebral body, steerability allows physicians to change trajectory simply by turning the gray handle of the PowerCURVE and Arcadia after accessing the vertebra.
This provides a targeted single-access ability to cross the vertebral midline, enabling optimal balloon tamp positioning and cavity creation. The steerable osteotome, when used alone, can provide targeted channel creation, simultaneously sparing healthy cancellous bone and maximizing surface area to facilitate cement interdigitation. In addition, targeted cavity creation supports the controlled delivery of high-viscosity cement with optimal cement fill.
Reduced Complications

The sophisticated steerable technology of the Arcadia system enables a unipedicular approach to treatment. Complications associated with vertebral augmentation, in general, include infection, neural damage, and pedicle fracture.6 Passing the spinal canal only once, as seen with a unipedicular approach, may reduce the occurrence of such complications.
The Arcadia Balloon-Assisted Vertebral Augmentation System is a prime example of the new technologies Merit provides physicians, helping them to improve procedural outcomes and better the patient experience.
Explore the Arcadia by visiting its product page or through the Merit Customer Support Center.
References
- Pilitsis JG. n.d. “Vertebral Compression Fractures.” https://www.aans.org/en/Patients/Neurosurgical-Conditions-and-Treatments/Vertebral-Compression-Fractures.
- Sun H et al. 2016. “Can Unilateral Kyphoplasty Replace Bilateral Kyphoplasty in Treatment of Osteoporotic Vertebral Compression Fractures? A Systematic Review and Meta-Analysis.” Pain Physician 19, no. 8 (Nov–Dec): 551–563. PMID: 27906934.
- Kudo K et al. 2003. “Anterior Spinal Artery and Artery of Adamkiewicz Detected by Using Multi-Detector Row CT.” American Journal of Neuroradiology 24(1): 13–17. PMID: 12533320.
- Liu L et al. 2019. “An Anatomical study on lumbar arteries related to the extrapedicular approach applied during lumbar PVP (PKP).” PLoS One 14, no. 3: e0213164. PMID: 30835754.
- Chung HJ et al. 2008. “Comparative Study of Balloon Kyphoplasty with Unilateral Versus Bilateral Approach in Osteoporotic Vertebral Fractures.” Int Orthop 32, no. 6 (Dec): 817–820. PMID: 17768624.
- Tsoumakidou G et al. 2017. “CIRSE Guidelines on Percutaneous Vertebral Augmentation.” Cardiovascular and Interventional Radiology 40(3): 331–342. PMID: 28105496.
Lessons from A Specialty Surgery Division at the Pandemic Epicenter
In March 2020, following a national emergency declaration, New York City was an epicenter of COVID-19. At Columbia University Medical Center, one department’s adaptive response “Reporting for Duty: Lessons from A Specialty Surgery Division at the Pandemic Epicenter,” was recently published in the Annals of Surgery.
The disruption to normal hospital operations was unprecedented and immediately posed two challenges: managing existing hospitalizations and a massive influx of COVID-19 patients. A third challenge emerged: caring for patients who were scheduled for surgeries that would inevitably be delayed.
The specialty surgery division implemented a rapid response strategy for breast surgical patient management with the SCOUT® Radar Localization System. SCOUT enabled the division to triage patients and prepare for downstream radiology backlogs, effectively managing the myriad of unprecedented challenges that COVID-19 imposed.
Highlights from the Annals of Surgery article include:
- Postponement of screening mammography enabled radiologists to perform SCOUT localizations to minimize downstream scheduling obstacles for surgical patients.
- SCOUT reflectors were placed, up to 10 localizations a day to prepare for surgical intervention. This approach allowed for flexibility with an operative schedule that was unpredictable. Localized patients could be added to the surgery schedule immediately if the Surgical and Procedural Scheduling Committee’s approval was obtained. Columbia University Medical Center did not need to default to wire localizations during the height of COVID management.
Recognizing Lung Cancer Awareness Month
November is Lung Cancer Awareness Month, an important time for us at Merit Medical. As a patient-centric healthcare company, it is our goal to not only provide the tools physicians need to treat and improve outcomes for lung cancer patients but also to share knowledge and increase awareness surrounding the disease.
WHAT IS LUNG CANCER?
Lung cancer is a type of cancer that begins in the lungs. It is the leading cause of cancer deaths worldwide.1 Among women in the US, it has surpassed breast cancer, becoming the leading cause of cancer deaths nationally.2
There are different kinds of lung cancer, but the two main types are non-small cell lung cancer (NSCLC) and small cell lung cancer (SCLC).3
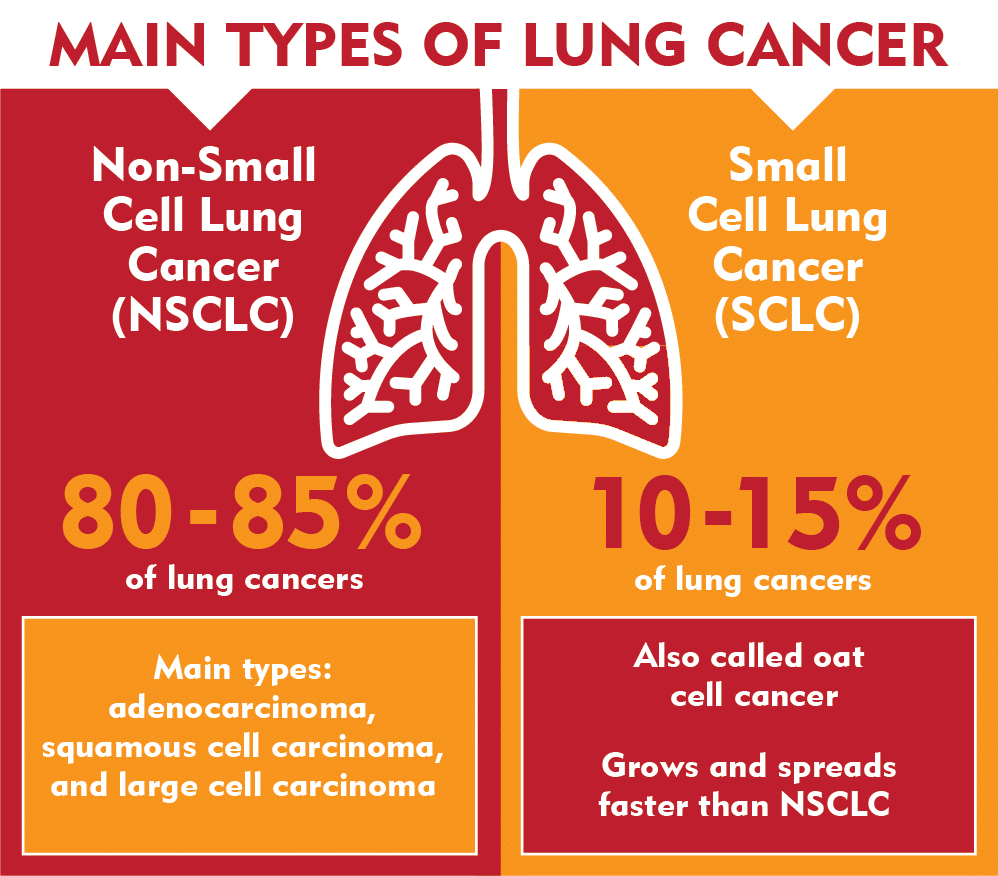
Learn more about NSCLC, SCLC, and other types of lung tumors here.
WHAT CAUSES LUNG CANCER?
It is unknown what causes every case of lung cancer, but there are known risk factors.
SMOKING4

Smoking is the leading cause of lung cancer, resulting in about 80% of lung cancer deaths. Although smoking is the strongest risk factor, it can also interact with other factors or not be the cause at all.
CAUSES IN NON-SMOKERS1,4
Many people who develop lung cancer are smokers or former smokers, whereas others have never smoked at all. Lung cancer in non-smokers can be caused by exposure to different substances, such as radon, secondhand smoke, air pollution, asbestos, diesel exhaust, and other chemicals. People with a family history of lung cancer are also at an increased risk.
A small percentage of people develop lung cancer who have no known risk factors. This may happen with no outside cause or may be due to factors we have not found yet.
Learn more about lung cancer risk factors as well as gene changes that may lead to the disease.
SYMPTOMS OF LUNG CANCER
In the early stages, lung cancer typically does not cause any signs and symptoms. In the advanced stages, common signs and symptoms of lung cancer can include:
- A new, persistent cough
- New onset of wheezing
- Coughing up blood or rust-colored phlegm
- Shortness of breath
- Chest pain, especially when breathing deeply, laughing, or coughing
- Hoarse voice
- Weight loss without trying
- Loss of appetite
- Fatigue
- Fluid in the chest
- Persistent infections, such as bronchitis and pneumonia
- Cancer spreading to other parts of the body (This can cause other signs and symptoms, such as headache, nausea, pain, etc., depending on which organ is affected.)
LUNG CANCER PREVENTION
Although lung cancer cannot always be avoided, steps can be taken to reduce your risk1.

Quit Smoking (or Don’t Start)
If you have never smoked, don’t start. If you want to quit, there are many replacement products, support programs, and medications available to help. Talk to your doctor.
Stay Away from Secondhand Smoke
Avoid places where people smoke. If you live with a smoker, encourage him or her to quit and ask that smoking be done outside.
Test Your Home for Radon
IIf you learn that you have high radon levels in your home, it can be corrected. Contact your local department of public health for more information.
Avoid Cancer-Causing Chemicals
Always follow precautions in the workplace to avoid toxic chemical exposure. If you work regularly in a hazardous environment, talk with your doctor to see what else you can do to protect yourself.

Live a Healthy Lifestyle
Choose a diet full of fruits and vegetables. Always choose nutritious foods versus taking large doses of vitamins, as some vitamins have been found to increase the risk of lung cancer.6 Include physical activity in your routine. Find a type of exercise you enjoy and try to be active most days of the week.
WHEN TO SEE A DOCTOR
If you notice any signs or symptoms that worry you, make an appointment with your doctor. If you need help quitting, your doctor can create a care plan that may include medication, counseling, support groups, online resources, and replacement products.
Only 16% of lung cancer cases are diagnosed at an early stage, and more than half of people with lung cancer die within one year of diagnosis.2 If you are at an increased risk of lung cancer, talk to your doctor about lung cancer screening options. Early detection can make a difference. The five-year survival rate for lung cancer is 56% for cases detected when the disease is still localized within the lungs.2 However, these rates decrease dramatically to only 5% when tumors have spread to other organs.2
At Merit, our goal is to help people worldwide live their best lives. Learn about the trusted interventional and palliative treatment alternatives we offer.
RELATED PRODUCTS
References
- Mayo Clinic. “Lung Cancer Symptoms and Causes.” Accessed October 23, 2020. https://www.mayoclinic.org/diseases-conditions/lung-cancer/symptoms-causes/syc-20374620
- American Lung Cancer Association. “Lung Cancer Fact Sheet.” Accessed October 27, 2020. https://www.lung.org/lung-health-diseases/lung-disease-lookup/lung-cancer/resource-library/lung-cancer-fact-sheet
- American Cancer Society. “What Is Lung Cancer?” Accessed October 23, 2020. https://www.cancer.org/cancer/lung-cancer/about/what-is.html
- American Cancer Society. “What Causes Lung Cancer?” Accessed October 23, 2020. https://www.cancer.org/cancer/lung-cancer/causes-risks-prevention/what-causes.html
- American Cancer Society. “Signs and Symptoms of Lung Cancer.” Accessed October 23, 2020. https://www.cancer.org/cancer/lung-cancer/detection-diagnosis-staging/signs-symptoms.html
- Mayo Clinic. “Drugs and Supplements Beta Carotene (Oral Route). Accessed October 23, 2020. https://www.mayoclinic.org/drugs-supplements/beta-carotene-oral-route/precautions/drg-20066795
Merit Medical Receives Supplier Horizon Award from Premier Inc.

Merit Medical is proud to be a 2020 Recipient of the Supplier Horizon Award, presented by Premier Inc., a leading healthcare improvement company that unites an alliance of more than 4,100 U.S. hospitals and health systems and approximately 200,000 other providers and organizations to transform healthcare.
One of only nine suppliers to receive the award this year, Merit was recognized for its oncology division’s support of Premier members through exceptional local customer service and engagement, value creation through clinical excellence, and commitment to lower costs.
Merit Oncology’s leading technology is SCOUT® Radar Localization, an advanced wire-free radar localization system designed to improve the precision and predictability of marking tumors, biopsy sites, and lymph nodes prior to neoadjuvant therapy and surgery. SCOUT Radar Localization is the wire-free platform that exclusively spans the care continuum from biopsy to surgery.
Used in more than 770 hospitals, October 2020 marked a milestone for SCOUT, as more than 150,000 women have experienced a wire-free localization.
Related News

Our Commitment. Our Promise.

Merit Medical is committed to reducing the burden that cancer places on patients and their loved ones. To further demonstrate this commitment, Merit is partnering with BreastCancer.org, an organization dedicated to educating and empowering people with breast cancer.
Throughout the months of September and October 2020, Merit will donate $1,000 to Breastcancer.org for each SCOUT® console sold worldwide that exceeds monthly goals. Learn more about SCOUT Radar Localization.
Like Merit, BreastCancer.org is committed to the mission of reducing the burden of breast cancer and reaches millions of people each month worldwide, providing much-needed resources and support.

During Breast Cancer Awareness Month and every month, Merit’s promise remains the same—to consistently invest in improving technologies and innovating new platforms that meet patient and physician needs.








![ReSolve® Biliary Locking Drainage Catheter [Introduction]](https://meritlegacy.decort.co/wp-content/uploads/2021/11/2021-11-23_12-22.png)