Mile-Markers to Breast Cancer Recovery with SCOUT®: The Tara Zuzga Story
Merit Medical is committed to reducing the burden of breast cancer on patients and their loved ones—patients like Tara Zuzga.

Working in the healthcare industry and having a family history of breast cancer, Tara knew that early detection saves lives. Throughout her life, she diligently underwent regular mammograms and ultrasounds. For a mass like this, however, she couldn’t wait for her next exam. With the support of her husband, who also works in the medical field, Tara connected with Dr. Blumencranz, a breast cancer specialist.
With an accurate diagnosis of breast cancer, she started chemotherapy two weeks later.
AN EXCELLENT CANDIDATE FOR SCOUT®

With Dr. Blumencranz’ help, Tara set off on her journey toward recovery. But she didn’t let her diagnosis slow her down, and she made sure every moment counted.
Tara and her husband continued having special date nights the evening prior to her bi-monthly chemo treatments. “He would take me out just to appreciate that moment before the next morning,” said Tara. “Which was a big deal.”
“She’s like super woman. She’d have her chemo, and then she’d go out walking,” reflected Tara’s husband. “All in all, she was the warrior in all of this.”
YOU’RE NO LONGER MY PATIENT
In January of 2022, Tara received the news she’d been hoping for.
She was cancer-free.
“The day Dr. Blumencranz told me, ‘You’re no longer my patient,’ we both stood there and cried,” said Tara. “When they say we’re checking you out, it’s a really big deal. It’s as big of a deal as ringing the bell for your last chemo. Those mile-markers are everything.”
Watch Tara’s journey to becoming cancer-free.
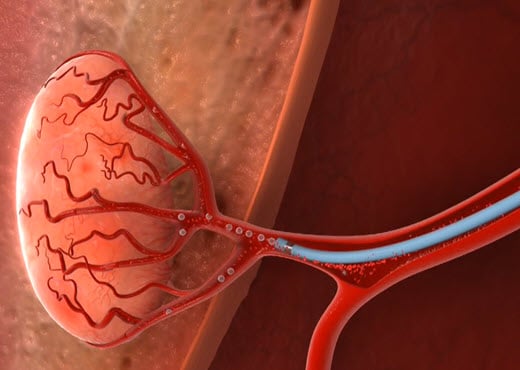
Becoming Fibroid Free: Malin Finds Relief Through UFE
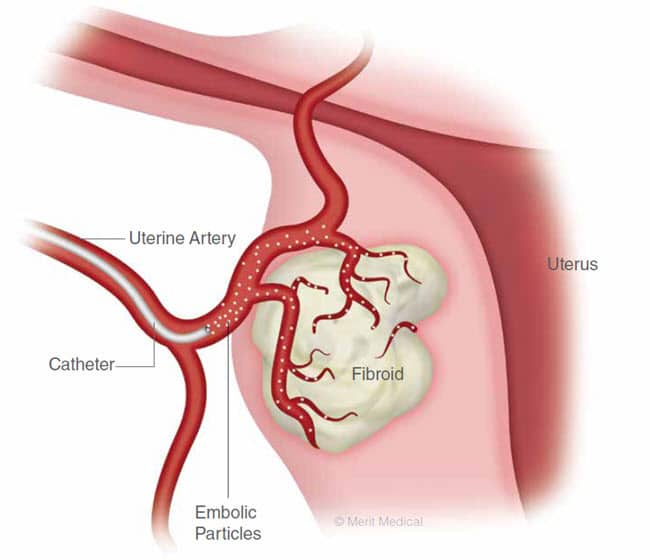
Two in three women will develop fibroids at some point in her life. Uterine fibroids are small, noncancerous growths that form on the wall of the uterus. Although benign, and while many women may not experience complications, for some, fibroid symptoms can be devastating. Worse, information on treatment options is not always made readily available, and many patients are led to believe that the only solution is major surgery—like a hysterectomy.

“Being 28, I found it really shocking that they said it was absolutely the only option,” reflected Malin. “I decided not to do it and learn how to live with my problems.”

As an employee of Merit Medical, Malin was familiar with uterine fibroid embolization (UFE). An alternative method of treating fibroids, UFE allows patients to preserve the uterus by stopping blood flow to the fibroids, which causes them to shrink—thus relieving symptoms.
For Malin, this presented an ideal solution. “I don’t want to remove an organ if I don’t absolutely have to,” she said. “I looked for someone to help me understand if I was a good candidate for UFE or not.”
Malin made a full recovery from the successful UFE procedure. With her symptoms gone or significantly reduced, she was able to get back to the activities she enjoyed prior to developing fibroids. “It’s like a new life,” she said.
These days, Malin spends her time advocating for increased awareness of UFE as a treatment option to help reduce the stigma around talking about fibroids. “Who would I be if I couldn’t stand up and tell my story? We have to start understanding and listening to each other.”
A New Lease on Life with Aspira®: The Andrea Peterson Story
Merit Medical is proud to support health at every stage, committed to helping patients live life to the fullest. For Women’s Health Week, meet Andrea Peterson—an advocate for adventurous women everywhere and patients who refuse to let a diagnosis slow them down.

“I just started living,” Andrea explained, recounting how her new outlook motivated her to become a firefighter, pilot, pianist, world-traveler, and more.
“It’s a beautiful world. I met people and had experiences that ordinary people don’t.”
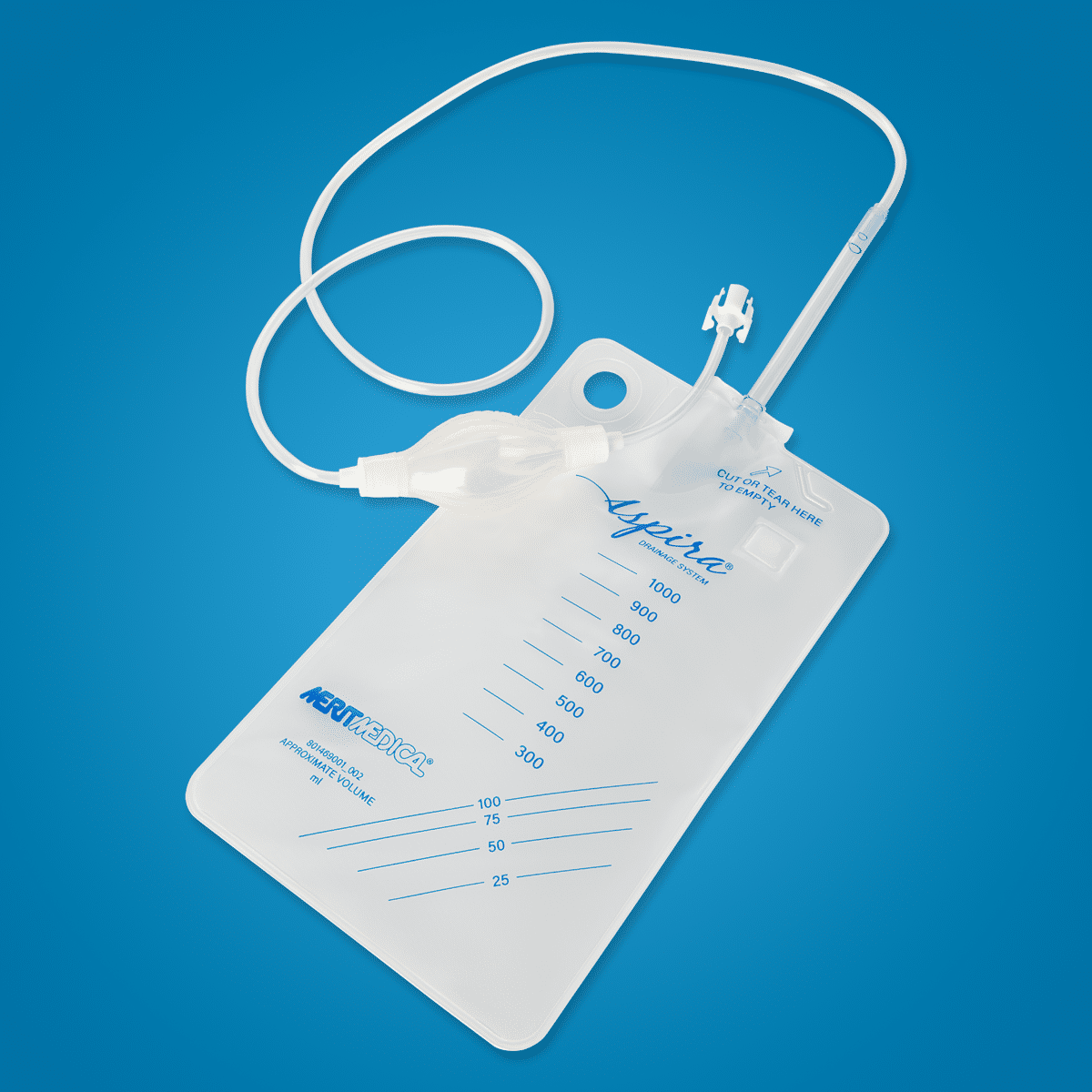
For Andrea, this was only her next great adventure. Because the Aspira system is designed to provide patients with maximum freedom, Andrea remarked, “I can still live and do anything I want. Every time we get a delivery of Aspira, it’s more life, more freedom, and more adventures.”
Andrea’s most recent expedition took her to Antarctica, a dream she’s pursued since childhood. And at her side? Her “freedom friend,” the Aspira bag.
Watch her full story.
Breast Cancer Awareness Month 2022

Merit Medical is committed to reducing the burden that cancer places on patients and their loved ones. During Breast Cancer Awareness Month, we are proud to partner with and support Living Beyond Breast Cancer, a non-profit organization whose mission is to connect people with trusted breast cancer information and a community of support. The LBBC fund specializes in providing underserved communities direct access to care via financial assistant grants.
We are excited to be the first and only surgical oncology company to partner with Living Beyond Breast Cancer. Our partnership with this organization will directly help underserved communities across the nation get the financial help and resources they need to navigate through this difficult time.

— Jean Sachs, CEO, Living Beyond Breast Cancer
SCOUT® Reaches a New Milestone During
Breast Cancer Awareness Month

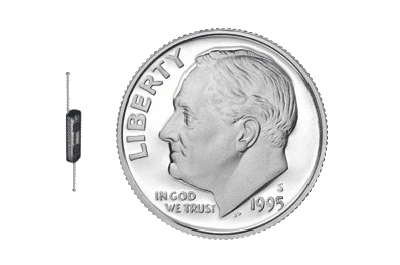
With more than 350,000 women experiencing wire-free localization with SCOUT, Merit’s promise remains the same—to consistently invest in improving technologies and innovating new platforms that meet patient and physician needs. See how SCOUT is improving the lives of patients all around the world.
Merit Medical Employee Support
The Merit team will also be honoring Breast Cancer Awareness Month worldwide during October.
Check back throughout the month of October and see how employees are contributing to this important cause!

The Aliso Viejo team celebrated BCAM with the annual luncheon, pink Merit shirts and pink smoothies this year. 😊

Our Merit team from Bogotá, Colombia, recently launched SCOUT Radar Localization and is very excited to offer this incredible product to Colombian patients.


At Merit, it’s all about family. Yuma Medina, Merit Technician III, and mom, Osleida Ferrer Rojas, Merit Operator II, show their support for #BCAM by wearing pink together! Thank you for the positivity you bring to our team!
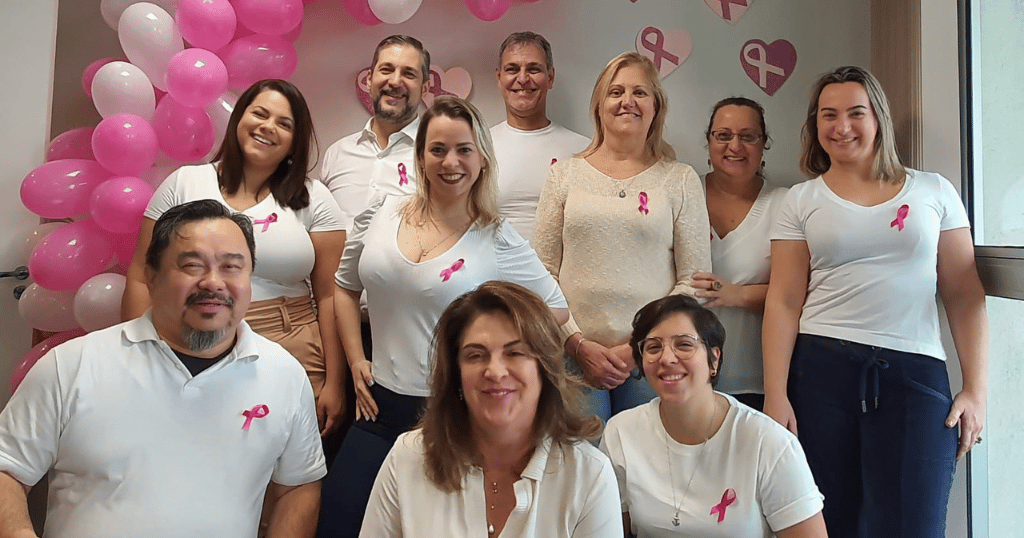
In honor of #BreastCancerAwarenessMonth, our Merit Brazil team coordinated a Pink Out day! We love seeing our global family reflect our commitment to raise awareness and empower people with breast cancer. Nice job, Brazil!

Our Merit Salt Lake Weekend Cleanroom Team is “thinking pink” in recognition of #BreastCancerAwarenessMonth! Thank you to Carina Gonzalez, Cleanroom Supervisor I, for rallying the team!


Meet Rebeca Mortimer, a Merit employee and #BreastCancerSurvivor. By coaching fellow fighters with optimism and compassion, she’s committed to spreading her story to raise awareness of this disease. You’re an inspiration, Rebeca! 💪


Merit Richmond is recognizing #BreastCancerAwarenessMonth, wearing pink as a team to raise awareness and honor those we’ve lost to breast cancer and survivors still with us. A reminder that when we come together, anything is possible.
#WeCare #TeamMerit





It’s #breastcancerawarenessmonth💕
In recognition of Breast Cancer Awareness Month, Merit Galway have donned their pink attire in support of those affected by breast cancer.
The #mariekeatingfoundation was on site and a GP lead cancer awareness seminar were available to all who wished to avail.
A cake sale was organised by our Sports and Social Committee today and tomorrow, to help raise money which will go towards life-changing research and support the amazing work carried out by, National Breast Cancer Research Institute, University Galway.
It’s days like today, we are reminded how kind our employees are!
To all the bakers who made yummy treats for the cake sale and to those who volunteered and donated so generously, Thank You!
Well done team!! 👏 #WearItPink #BreastCancerAwareness #MeritGalway #Support #BCAM22 #WeCare


Merit Asia celebrated Breast Cancer Awareness Month with a variety of #PinkActivities for people of all fitness levels. We dressed up in PINK for #PinkWalk, #HIIT, and even #Picnic!🚶🏻♀️
Whichever we choose, physical exercise and activity are advantageous in reducing the risk of breast cancer. Merit is committed to reducing the burden that cancer places on patients and their loved ones. ❤️ 💪🏻 These are meaningful activities for a worthy cause! #TeamMerit #WeCare #BreastCancer #BreastCancerAwarenessMonth




Closing this Pink October with a great team ! In recognition of #breastcancerawarnessmonth, we would like to thanks everyone for your support in your daily work by providing devices which improve patient quality of life. #Paris #PinkOctober #2022

Carmen’s Journey with Fibroids and Finding Relief in UFE

Although some women with fibroids have no symptoms, others may experience abdominal pain, frequent urination, enlargement of the lower abdomen, and heavy menstrual bleeding.2 Despite its prevalence and severe symptoms, the condition is seldom discussed. To change that, we talked with Carmen McKeever, who was first diagnosed with uterine fibroids during an appointment with her gynecologist.

“Fibroids really impacted my everyday life.” Carmen explained. “Professionally, I am a nurse. At my facility, our uniform is white scrubs. So you can imagine, every month it was like a nightmare.”
During her period, Carmen had to equip herself with an “arsenal” to make it through the day and avoid accidents. On any given day, she admitted to needing a super absorbency tampon, two ultra-absorbency maxi-pads, a Depend® adult diaper, and Spanx® to hold it all together.
All of this wasn’t enough, as Carmen explained. “I also had all that stuff in my bag just in case I had to change, which was about every hour.”
Unable to tolerate going through life like this any longer, Carmen explored fibroid treatments. But like other women seeking an alternative to a complete hysterectomy, Carmen faced resistance when meeting with doctors.
“The help I received from medical professionals was—operate. Hysterectomy. That was it. I just felt like I was being dismissed,” she recalled with emotion. “I oftentimes felt like it was my fault that I had fibroids. That I was wasting people’s time because I was trying to figure out what I was going to do, and not have a hysterectomy, and that was the only answer I was getting.”
After searching and getting nowhere, Carmen finally learned about uterine fibroid embolization (UFE) from an acquaintance who also suffered from fibroids. After attending a free UFE hospital seminar presented by Dr. John Lipman, a vascular and interventional radiologist and fibroid specialist at Atlanta Interventional Institute, she was intrigued.
Upon meeting with Dr. Lipman and learning of UFE, Carmen felt at ease. “He made sure that I had all the information and that I was well-informed, so I could make a logical decision.”
Carmen decided to get UFE and felt it was the best decision. “My pain [during recovery] was nothing compared to the menstrual cramps that I experienced every month,” she described. After resting for four days, she returned to work just one week after the procedure.

Hear from more patients who have overcome fibroids with UFE and now live full, healthy lives.
The above information should not be construed as providing specific medical advice but rather to offer readers information to better understand their lives and health. It is not intended to provide an alternative to professional treatment or to replace the services of a physician.
REFERENCES
- U.S. Food & Drug Administration. “Knowledge and News on Women: Fibroid Awareness Month”. July 1, 2021. https://www.fda.gov/consumers/knowledge-and-news-women-owh-blog/knowledge-news-women-fibroid-awareness-month
- U.S. Department of Health and Human Services. Office of Women’s Health. “Uterine Fibroids”. February 19, 2021. https://www.womenshealth.gov/a-z-topics/uterine-fibroids
Men’s Health Month: Reclaiming Quality of Life with Prostatic Artery Embolization

We sat down with Larry Sago, a patient who underwent PAE, to hear his story and better understand how life changing the procedure can be.
“The difference is like night and day,” Larry said, describing his life before and after prostatic artery embolization (PAE).
Larry’s journey began when he was diagnosed with BPH. A common condition, about half of all men in their 50s develop BPH—a statistic that increases with age.1 Although non-cancerous, BPH can cause a host of bothersome urinary symptoms, including feelings of urinary urgency, weak or interrupted urine stream, and urinary frequency.

For many men like Larry who suffer from BPH, the first line of treatment is commonly prescription medications to treat the symptoms, but these are occasionally ineffective and often have less-than-desirable side effects. After trying medications, Larry found his symptoms couldn’t be controlled any longer and continued to worsen. “My urologist told me TURP [transurethral resection of the prostate] was about the only answer.”
TURP is a surgical procedure that cuts away the prostate tissue that blocks the flow of urine. While very effective in improving urination, it can be associated with complications like bleeding, urinary leakage, and sexual side effects. The bleeding risks become more concerning the larger the prostate becomes.
Not wanting to have surgery or to risk having the complications associated with TURP, Larry researched non-surgical treatment options online but wasn’t finding much. As luck would have it, Larry one day found an article by University of North Carolina (UNC) Clinical Assistant Professor of Radiology Dr. Ari Isaacson discussing minimally invasive PAE at the UNC Health Care System’s Center for Heart and Vascular Care.
“I emailed Dr. Isaacson as soon as I read about [PAE],” Larry recalled. “Amazingly, within half an hour he’d written me back asking for my phone number to further talk about the procedure. He called me and communicated all aspects of [PAE] very clearly.” Liking what he heard, Larry drove from Atlanta to Chapel Hill to meet with Dr. Isaacson. Once a biopsy cleared him of prostate cancer, Larry was able to undergo the procedure as part of a clinical trial.
PAE is performed by an interventional radiologist and takes approximately one to two hours to complete. Under conscious sedation, a small puncture is made in the upper thigh or arm. A slender catheter is then inserted and guided via real-time imaging into the prostatic arteries that supply the prostate with blood. Tiny embolic particles are injected into these arteries, blocking blood flow to the enlarged areas of the prostate. Once deprived of blood, these areas of tissue die (necrosis).
“PAE results in shrinking and softening of the prostate which allows for urine to flow through easier, ultimately reducing urinary symptoms,” Dr. Isaacson explained. “Some of the advantages of PAE are that it is performed as an outpatient procedure, and the recovery time is quick. In most cases, no Foley catheter is required. PAE also has very little chance of affecting sexual function. In some cases, sexual function is even improved after patients are able to stop taking BPH medications.”
Post-PAE, Larry describes the procedure as easy with no pain or bleeding. Afterward, he was able to go back to his hotel room in Chapel Hill, spend the night, and drive home to Atlanta the next day. “For about a week, my former BPH symptoms returned, but they were briefer and milder this time. Once they went away, I felt like I was 20 years old again!”
PAE not only resulted in clinical improvements, it also gave Larry something priceless—his life back.
“I literally don’t think about the symptoms I used to struggle with,” Larry said. “I can go play golf without having to worry about going to the bathroom in the middle of the golf course!”
Feeling truly fortunate to have been a candidate for PAE, Larry said the only thing he would’ve done differently was have the procedure sooner. “If this treatment had been available, I would’ve done it years earlier. I simply hope there’s more awareness so that others can experience the boost in quality of life and long-term health that I did.”
Explore other patient testimonials and learn more about PAE.
At Merit, our mission is to improve the lives of people, families, and communities around the globe. If Larry’s story resonated with you, and you’re experiencing bothersome symptoms from BPH, talk to your doctor today to see if PAE might be an option for you.
The above information should not be construed as providing specific medical advice but rather to offer readers information to better understand their lives and health. It is not intended to provide an alternative to professional treatment or to replace the services of a physician.
REFERENCES
- Urology Care Foundation. (n.d.). What Is Benign Prostatic Hyperplasia (BPH)? Retrieved from http://www.urologyhealth.org/urologic-conditions/benign-prostatic-hyperplasia-(bph)/
Breaking Down Osteoporosis with Dr. Altin Stafa

What is osteoporosis, and who is most at risk?
Some consider osteoporosis a “silent” disease, because people with osteoporosis typically do not learn of their diagnosis until first breaking a bone. Fractures can occur in any bone but are most common in bones of the hip, wrist, and vertebrae in the spine.
“Osteoporosis mainly affects women at menopause when levels of bone-bolstering estrogen fall rapidly,” Dr. Stafa explains. “However, it should not be forgotten that men of the same age, even though much less frequently, can also suffer from osteoporosis. In addition, pathological conditions, such as hyperparathyroidism and chronic kidney disease, can cause gender-independent osteoporosis even at a younger age.”
If a parent experiences a broken hip or other broken bone, one may be at higher risk and should discuss with a doctor if screening for osteoporosis is recommended.
What types of fractures are most common among patients with osteoporosis?

For some patients with more severe osteoporosis, Dr. Stafa shares that “the mid thoracic vertebrae can also fracture.” He advises giving special attention to the sacrum, that sits below the lumbar vertebrae, which frequently has underdiagnosed fractures. “Compression fractures of the cervical spine in the neck region and of the upper thoracic region are rare,” Dr. Stafa adds.
How are fractures diagnosed and treated?
People experiencing significant, sudden, localized back pain that interferes with daily life should consider seeking medical expertise to evaluate their spine for possible diagnosis of a vertebral fracture. “Even when they are not painful, osteoporotic vertebral fractures may cause a gradual and severe reduction of the vertebral body height, which can negatively impact the biodynamics of the whole spine, causing spinal deformity (i.e., kyphosis), chronic back pain, consequent chest and abdominal space reduction with overall negative impact on the patient’s quality of life,” Dr. Stafa explains.
A number of treatments are available for patients with fractures, according to Dr. Stafa. “Vertebral compression fracture treatments include pain medication, bed rest, and bracing as well as physiotherapy. Although these approaches may help some patients, most of them have found little to no relief or clinical improvement.”
What is vertebral augmentation treatment?
“People with serious pain from fractures may benefit from vertebral augmentation. This minimally invasive procedure has provided substantial, immediate pain relief while reducing progressive vertebral body height reduction and consequent spinal deformity,” Dr. Stafa explains. Vertebral augmentation involves one or two very small incisions in the skin (less than 1 cm in length) to access the vertebral body affected by the fracture, creating channels or cavities inside the vertebral body, and delivering bone cement to stabilize the fracture.


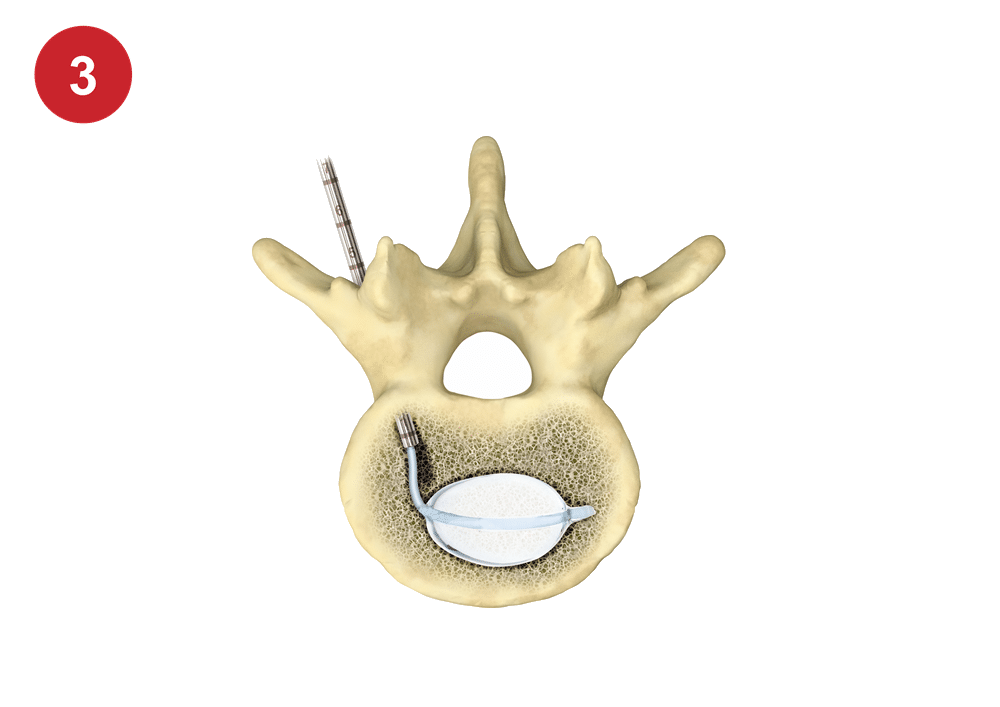
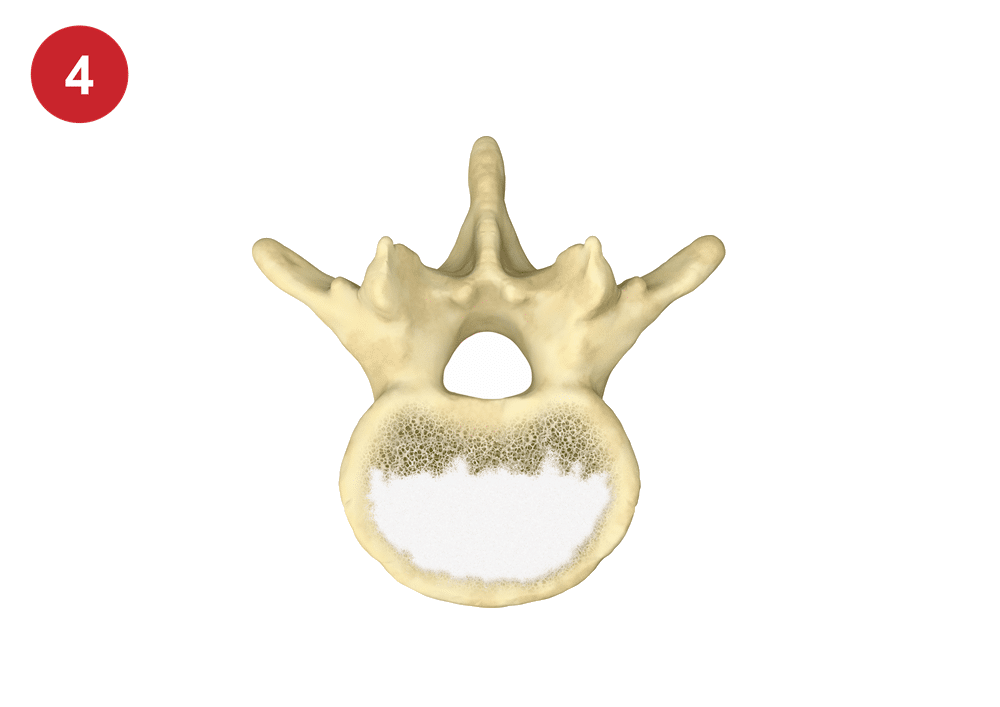
Merit has designed cutting-edge vertebral augmentation products for physicians that address patient-specific needs when treating vertebral compression fractures. “Good clinical outcomes are a result of the ability to control the size, shape, and location of channels and cavities in the vertebrae, using steerable devices, to allow for optimal amount and location of cement, to stabilize the fracture,” Dr. Stafa shares.
Merit Medical is dedicated to collaborating with physicians to innovate the tools needed to help create a better quality of life for people living with osteoporosis. Learn more about our Spine portfolio of diagnostic and interventional products that target spine pathology and reduce pain with minimally invasive precision. Contact our Customer Support Center to learn how you can implement these and more into your practice.
References:
- Centers for Disease Control and Prevention. 2022. “Does Osteoporosis Run in Your Family?” https://www.cdc.gov/genomics/disease/osteoporosis.htm
- National Institutes of Health. 2022. “Osteoporosis Overview.” https://www.bones.nih.gov/health-info/bone/osteoporosis/overview
Embosphere® Results in Less Inflammatory Response, Lower Rates of Analgesic Use Compared to PVA After UFE
Every July, our team at Merit Medical recognizes Fibroid Awareness Month as a time to bring attention to a very common yet under-discussed condition that will affect most women at some point in their lifetime.
We do this by supporting a minimally invasive fibroid treatment called uterine fibroid embolization (UFE), also called uterine artery embolization (UAE), through a portfolio of embolotherapy products we offer.
Published in Radiology, the study enrolled 54 women with fibroids (mean age, 44 ± 4 years [standard deviation]) and assigned UFE treatment with either nonspherical PVA (355–550 μm) or Embosphere (500–700 μm). There were 27 women in each group, and both participants and investigators collecting data were blinded to the embolic material used. Women with concomitant disease (e.g., adenomyosis) were excluded from the study.
Both groups were given fentanyl-based intravenous patient-controlled analgesia within the first 24 hours after UFE as well as rescue analgesics. The investigators measured neutrophil-to-lymphocyte ratio to assess inflammatory response, and contrast-enhanced MRI was performed 1 day after the procedure to evaluate dominant fibroid necrosis and ischemia of normal myometrium. Symptom severity score and health-related quality-of-life score were assessed before and 3 months after UFE.
Results showed that pain scores and fentanyl dose were not different during the first 24 hours, but the use of rescue analgesics was higher in the PVA group (33% vs 11%; P = 0.049). After embolization, symptom severity score and health-related quality-of-life score were not different between groups (symptom severity score: 16 [interquartile range, 6–22] for PVA vs 19 [interquartile range, 9–34] for Embosphere, P = .45; health-related quality-of-life score: 93 [interquartile range, 80–97] for PVA vs 89 [interquartile range, 84–96] for Embosphere, P = .41).
In addition, changes in neutrophil-to-lymphocyte ratio from before to 24 hours after UFE were greater in the PVA group (3.9 [interquartile range, 2.7–6.8] compared to the Embosphere group (2.5 [interquartile range, 1.5–4.6]; P = .02). Rates of complete dominant fibroid necrosis were not different between groups, but transient global uterine ischemia of normal myometrium was more frequent in the PVA group (44% vs 15%; P = .04).
The investigators of the study concluded that when used in UFE, PVA particles and Embosphere resulted in similar pain scores and fentanyl dose. However, PVA resulted in a greater inflammatory response, higher rates of rescue analgesic use, and more frequent transient global uterine ischemia compared to Embosphere.
Watch How UFE Works
Fibroids (also known as uterine fibroids, leiomyomas, and myomas) are non-cancerous tumors that grow within the muscle tissue of the uterus. Although some fibroids cause no symptoms at all, common symptoms can include excessive menstrual bleeding, pelvic pain and pressure, and frequent urination. Depending on the size and location of the fibroids, other symptoms can include anemia, leg pain, pain during sexual intercourse, constipation, and an enlarged abdomen. Up to 80% of women develop fibroids by the time they reach age 50.
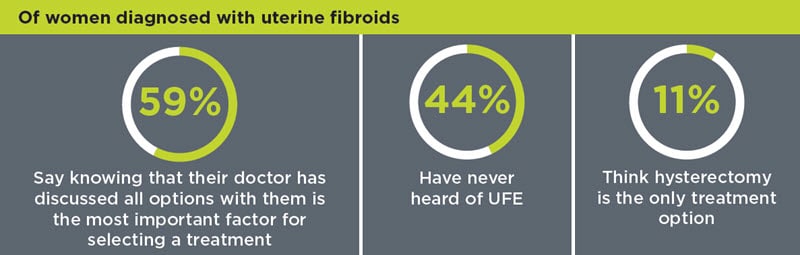
Approximately, 600,000 hysterectomies are performed in the US each year, with fibroids listed as the most common reason. A report by the Society of Interventional Radiology found that 1 in 5 women believe hysterectomy is the only treatment option for fibroids and that 44% of women with fibroids have never heard of UFE. Although hysterectomy is a treatment for fibroids, there are many other treatment options available, many of which are minimally invasive.
To encourage women to seek out all treatment options and help physicians educate patients, we offer an educational patient-awareness site called Ask4UFE with information about treatment options—with focus on UFE—as well as patient and physician testimonials and researched blog entries.
Join us in recognizing July as Fibroid Awareness Month. We look forward to working together to increase awareness surrounding the condition, helping to provide the best resources, products, and care for patients worldwide.
Before using, refer to Instructions for Use (IFU) for indications, contraindications, warnings, precautions, and directions for use.
ARTICLE REFERENCE
Han K et al. 2020. “Nonspherical Polyvinyl Alcohol Particles verusus Tris-Acryl Microspheres.” Radiology 298, no. 2 (Feb): 458–465. PMID: 33350893.
Merit Recognizes National Osteoporosis Month

Vertebral compression fractures, or VCFs, are the most common osteoporotic fracture—almost twice as common as other fractures caused by osteoporosis. Osteoporotic fractures can lead to long-term pain and even be life threatening.
1 in 3 Women & 1 in 5 Men Over 50 Years Old
To help care for this patient population, we provide a wide range of innovative tools for vertebral augmentation (kyphoplasty) and vertebroplasty treatments.
Listen in as Mrs. Steiner, a patient who suffered from a painful VCF, explains in her own words how treatment with Merit’s steerable Arcadia™ Balloon-Assisted Vertebral Augmentation System helped her resume an active lifestyle.
Browse helpful osteoporosis month resources:
- American Bone Health
- Bone Talk Podcast
- International Osteoporosis Foundation
- National Osteoporosis Foundation
- NIH Osteoporosis and Related Bone Diseases National Resource Center
RELATED PRODUCTS
Before using any of the Merit products mentioned above, refer to Instructions for Use for indications, contraindications, warnings, precautions, and directions for use.
“When You Are Informed, You Hold the Power” – Sharon Huff, SCOUT® Patient
“A close friend and I are going through this breast cancer journey together. She is a few weeks ahead of me in her diagnosis, so I have learned a lot from her experience,” Sharon said. “She had a wire localization and told me, in her words, it was going to freak me out. She had the wire put in very early the morning of her surgery and had to be still, so the wire wouldn’t move. Moving the wire could result in not being able to accurately locate the cancer.”
It came time for Sharon’s surgical consult with Dr. Jonsson at Kaiser Ontario Medical Center, and she was expecting to learn of her surgery date and hear about the wire localization procedure. This weighed heavily on Sharon’s mind. When Dr. Jonsson told her she would be having a wire-free localization, she was pleasantly surprised and relieved.
Although Sharon has an extensive educational background and is an avid reader and researcher, she had never heard of a reflector placement with SCOUT®. She immediately turned to the internet. Sharon read everything she could find about the procedure and watched videos to familiarize herself with what the reflector looked like and how it was placed.
When it was time for her reflector placement with Dr. Nguyen of the radiology department at Kaiser Fontana Medical Center, she was well informed and prepared. “The procedure to implant the reflector was easy and did not take long at all,” Sharon commented. “I was very impressed.”
COVID-19 adds additional stress to any medical procedure. In Sharon’s case, her husband was not allowed to accompany her and instead had to wait in the car. On the day of surgery, she only had to arrive two hours prior to the surgery start time, making her husband’s wait time much shorter than if she would have needed a wire localization on the day of surgery. “Having that little reflector made our day so much smoother and shorter,” Sharon recounted.

When asked to share pearls of wisdom for individuals going through the breast cancer journey, Sharon had three: inform yourself, make your own decisions, and advocate for yourself. “When you are informed, you hold the power,” Sharon said. “And you can feel better about your choices.”
Disclaimer: This information is not intended nor recommended as a substitute for medical advice, diagnosis or treatment. Always seek the advice of a qualified physician regarding any medical questions or conditions.
Updated Spine Resources for Your Practice

Merit Medical has recently updated its online Spine Resource Center as a way to support you in your spine practice as well as to help provide the best possible outcomes for patients undergoing vertebral augmentation (kyphoplasty), vertebroplasty, and spinal tumor ablation treatments. By inserting your email address, you’ll have access to a wide range of valuable tools and helpful information available for download.
Patient Education
Educate patients and increase awareness about interventional spine procedures with both digital and printed resources.
Digital Patient Resources
Use Merit’s digital tools on your practice website and social media as well as to boost your overall patient education efforts. With a licensing agreement, you’ll have access to treatment-related text, illustrations, and videos.
Printed Patient Resources
Order printed patient collateral, such as informational brochures and other patient awareness materials, simply by filling out an order form. The materials will be shipped to you at no cost.
Referring Physician Education
Collaborate with fellow physicians using Merit’s peer-to-peer presentations that address important topics, including patient selection, clinical evidence supporting interventional spine procedures, and more.
Clinical Resources
Throughout your day-to-day, take advantage of Merit’s many clinical resources. Product and procedure visual guides, disease management sheets, and prep and administration instructions are right at your fingertips.
Physician Support
To make your life easier, Merit provides updated coding and reimbursement information. A CMS Physician Fee Schedule look-up tool provides information for more than 10,000 physician services.
Data & Studies
Browse our list of key therapy studies that include quick links to abstracts and useful data summaries.
Merit Medical is committed to helping you care for your patients by offering the most up-to-date information available on interventional spine treatments. Visit the Merit Spine Resource Center today and explore the many tools you can use to enhance your practice.
Merit Addresses Growth in Home Dialysis Care with Patient and Physician Tools

There has been a recent shift in kidney care with both industry leaders and the White House showing support of home dialysis. This forward momentum is due to several advantages home dialysis offers patients, such as lower mortality rates,1 flexible treatment schedules,2 and reduced cost.3 Merit Medical is pleased to support this transition by providing dialysis patient education, clinician training, and a number of therapeutic products.
Heading the movement are international industry leaders DaVita® Kidney Care and Fresenius Kidney Care with an initiative called 20% by 2020, a program that aims to have 20% of dialysis patients on home dialysis therapy by the year 2020. Both DaVita and Fresenius provide two types of home dialysis options: peritoneal dialysis (PD) and hemodialysis.
“The initiative is important from several standpoints,” says John H. Crabtree, MD, general surgeon, chair of PD University for Surgeons-North America, and visiting clinical faculty at Harbor-UCLA Medical Center in Torrance, CA. “Number one, patients do better on home dialysis.”
Patients on PD therapy in particular, a group that comprises the majority of the home dialysis-treatment population, “have improved survival over the early years on treatment,” Dr. Crabtree told Merit Medical.4 Moreover, for individuals who receive a kidney transplant, “the results tend to be better when they were on peritoneal dialysis prior to the surgery as opposed to hemodialysis.”5
Home dialysis also offers greater autonomy. Because patients are properly trained and therapy can be done overnight, home dialysis allows for a regular work schedule.3 Moreover, the average cost of care for home dialysis is less.3 PD in particular, Dr. Crabtree went on to explain, is approximately $15,000 less per patient per year compared to hemodialysis.6
The White House recently announced a new government-sponsored payment approach for treating kidney disease that favors lower cost home dialysis. The U.S. Centers for Medicare and Medicaid Services is considering a trial program design that would improve care in the early stages of kidney disease, increase access to kidney transplants, and favor home dialysis over clinic-based treatment.3 It is particularly looking at the benefits of PD.3
Despite these advantages and the fact that many physicians believe 25%–35% of patients would do better on home dialysis therapy, the number of people receiving home dialysis in the US still remains low, with only 7% receiving PD and less than 1% choosing home hemodialysis.7 The 20% by 2020 initiative plans to change this through several avenues.
“The way that we can drive this is by improving patient education…Many patients aren’t provided information about home dialysis,” Dr. Crabtree explains. In addition to patient education, Dr. Crabtree says many physician education programs lack the training needed to take care of PD patients. “[I]t’s important to provide courses [and] educational opportunities that allow them to have hands-on training.”
Merit Medical is ready to address these needs through its Ask4PD™ patient education site and ThinkDialysisAccess™ hands-on physician training experiences. Merit also offers high-quality dialysis products, such as the Flex-Neck® Peritoneal Dialysis Catheter, a premium catheter that allows for up to 30% higher flow rates than other catheters currently on the US market.8
The support for home dialysis is expanding. By providing the tools and education needed to advance the 20% by 2020 initiative, Merit shows its ongoing evolution as a healthcare company as well as its vision to continually find ways to improve patient care.
Watch Dr. Crabtree’s interview to learn more about the benefits of home dialysis and how Merit supports it.
Dr. Crabtree is a paid consultant of Merit Medical.
REFERENCES
- DaVita® Kidney Care. (n.d.). Top 5 benefits of home dialysis treatment. Retrieved from https://www.davita.com/treatment-services/home-dialysis/home-benefits/top-5-benefits-of-home-dialysis-treatment.
- Fresenius Kidney Care. (2019). Learn more about home dialysis treatment options. Retrieved from https://www.freseniuskidneycare.com/ckd-treatment/benefits-of-home-dialysis.
- Copley, C., & Humer, C. (2019, March 3). U.S. seeks to cut dialysis costs with more home care versus clinics. Retrieved from https://www.reuters.com/article/us-usa-healthcare-dialysis/us-seeks-to-cut-dialysis-costs-with-more-home-care-versus-clinics-idUSKCN1QL0G6.
- Teixeira, J.P., Combs, S. A., & Teitelbaum, I. (2015). Peritoneal dialysis: Update on patient survival. Clin Nephrol, Jan;83(1):1-10.
- Joachim, E., Gardezi, A. I., Chan, M. R., et al. (2017). Association of pre-transplant dialysis modality and post-transplant outcomes: A meta-analysis. Perit Dial Int, May-Jun;37(3):259-265.
- United States Renal Data System. (2018). 2018 annual data report (Chapter 9: Healthcare expenditures for persons with ESRD). Retrieved from https://www.usrds.org/2018/view/v2_09.aspx
- DaVita Kidney Care. (n.d.). Majority of nephrology professionals prefer home dialysis. Retrieved from https://www.davita.com/treatment-services/home-dialysis/recommended-approach.
- Data on file.