Notable Awards and Recognitions in 2021

Each award received is a testament to our mission of improving the lives of people, families, and communities throughout the world. Whether it was through the actions we took to reduce our environmental footprint or protocols put in place to keep our employees safe during the pandemic—2021 was a year of perseverance and determination to make a difference.
Utah Business 2021 Green Business Award
Merit’s global headquarters in Salt Lake City, UT, received the 2021 Green Business Award, which recognizes organizations and individuals making positive strides to promote sustainability within the Utah community. Merit specifically won in the Corporate Initiative category for the actionable steps taken to reduce the company’s environmental footprint, now and in the future:
 Designing an Environmental Management System
Designing an Environmental Management System
As a global manufacturer of medical devices, Merit plays a significant role in contributing to a sustainable future. Sound environmental practices are beneficial to our employees, our customers, and the patients whose lives benefit from our products. Our Environmental Management System is designed to measure, monitor, and facilitate continuous improvement to ensure we meet our sustainability goals. This includes:
- Diverting waste from landfills by recycling materials, such as metal, plastic, wood, and cardboard
- Eliminating additional shipping materials through our Merit Smart Shipping™ program
- Supporting an on-site garden to reduce the amount of produce shipped to our facility
- Striving for a zero-food-waste policy
Looking Forward
As a leader in the healthcare industry, we have implemented specific goals centered around combating climate change and reducing our usage of water resources. Learn more about our commitment to a sustainable future here.
By building on our past successes and taking the initiative to improve year over year, we aim to positively impact both communities in Utah and around the globe.
The Stevie® Awards for Frontline Medical Hero of the Year
This year Dr. Nicole Priest, Chief Wellness Officer at Merit, won gold in the Stevie Awards for Frontline Medical Hero of the Year for her efforts in mitigating the effects of the COVID-19 pandemic at our Merit facilities worldwide.
When the COVID-19 pandemic began, Dr. Priest was instrumental in innovating safe ways to enable employees to continue working. In addition to enforcing social distancing and mask guidelines before state and federal mandates were established, Dr. Priest ensured that educating employees on safe pandemic practices was a top priority. Through bi-monthly Wellness Newsletters, she provided case updates, healthy lifestyle guidance, and information as the pandemic unfolded.
She also partnered with the Salt Lake Health Department to bring vaccine education sessions directly to our campus, and in May of 2021, the Merit Care clinic began offering the COVID-19 vaccine to all employees and their dependents, creating an accessible avenue to help stop the spread of the virus. Thanks to Dr. Priest’s efforts, Merit was able to continue operations safely and efficiently throughout 2020.
Utah Business 2021 Healthcare Heroes

From the onset of the pandemic, Mr. Lampropoulos was quick to adapt Merit’s strategy to ensure employees were able to safely continue producing the life-saving medical devices the company is known for. By working closely with Dr. Nicole Priest, Chief Wellness Officer at Merit, Mr. Lampropoulos ordered and implemented COVID-19 safety measures, including mask mandates, social distancing, and temperature screening for employees on campus, and instructed many departments to move to a work-from-home solution where possible.
In order to further support employees during this uncertain time, Mr. Lampropoulos developed new travel policies, approved a pandemic sick leave policy, and began providing free meals to Merit employees working on campus through the on-site cafeteria. Thanks to his commitment to his employees, their families, and the communities we serve, Merit was able to continue designing, manufacturing, and shipping essential medical devices while maintaining employee morale during the pandemic.
These great achievements are the result of our dedicated teams working every day to make a difference. Thank you, Team Merit! We look forward to seeing what we accomplish in 2022!
2021 Merit Garden Accomplishments

With another garden season successfully completed, it’s time to reflect on how we’ve grown in 2021 — and helped our team, our community, and our environment flourish in the process.



Employee Participation
2021 saw record numbers for many of our garden programs.
50 DIVISIONS
With 190 employees representing 50 different Merit departments, our garden box program was a huge success. Employees enjoyed a record year of produce to take home to their families.
562 VISITS
Our U-Pick program, where employees can select their own basket of fresh produce in exchange for 10 minutes of volunteer gardening, drew 260 employees from 73 Merit departments, totaling 562 visits in all.
5,400 POUNDS
Merit team members who participated in U-Pick enjoyed 5,400 pounds of delicious and healthy fresh fruits, veggies, and herbs. That’s 2,400 pounds more than 2020!
Garden Fresh Goods
Our gardeners certainly have green thumbs, and our employees enjoyed the rewards.
- 13,000 plants thrived in the Merit greenhouse — 4,500 of which were purchased by Merit employees.
- 210 cut flower arrangements were purchased by employees to brighten up a room or bring joy to a loved one.
- 2,500 pounds of produce was prepared into delicious meals in our Merit Salt Lake employee cafeteria.
- 2,000 plants were grown to be used by our Salt Lake landscaping team.

Giving Back
Philanthropy and charity are part of what makes Merit great. The Employee Garden is just one avenue for giving back to our community.
Garden sales generated $15,000 for the Candy Cane Program, helping employees in need have a brighter holiday season.
640 pounds of produce was donated to low-income senior centers.
400 surplus vegetable starter plants were donated to a local Title I school, where they were planted in their community garden and distributed to families to plant at home.
2,500 pounds of surplus produce was given away to Merit employees at the community garden table.
Going Green
Merit’s commitment to sustainability includes our garden efforts, too.
- 6 tons of green waste was taken to the Trans-Jordan landfill to make compost.
- All inedible produce was donated to feed farm animals at Roots Charter School, a nonprofit alternative high school in Salt Lake City.
See Our Year in Photos
For a closer look at what our garden is up to, watch this video of pictures taken throughout the year.
None of these achievements would be possible without our dedicated Employee Garden team. Thank you! We can’t wait to see what will grow in 2022.
For more information on how Merit works to improve the lives of employees, take a look at our Employee Wellness, Health, and Safety page.
Building a Culture of Inclusivity: Merit Welcomes the Women’s Leadership Initiative
To maintain this commitment to promoting inclusivity, Merit is proud to introduce the Women’s Leadership Initiative (WLI). As the first-ever affinity group at Merit, the WLI brings multiple benefits to members and strengthens Merit’s overall company culture.
The Women’s Leadership Initiative
Tracy Wood
VP of Strategic Accounts
Chairperson of WLI
The Women’s Leadership Initiative (WLI) offers professional growth, networking, opportunities for personal and professional enrichment, such as mentoring, professional and leadership development, career evolution, and community-involvement activities.
“It’s about promoting a culture of inclusion,” says Tracy Wood, Vice President of Strategic Accounts at Merit and chair of the WLI. “Our goal is to cultivate growth by sharing perspectives, allowing colleagues to network, and facilitating additional professional development opportunities to help further people’s careers with Merit.”
As an affinity group—an employer-recognized collection of individuals who share similar interests and goals, such as encouraging inclusivity and diversity—the WLI hopes to enhance the Merit experience for all employees.
Affinity Group Advantages: Diversity is Essential to a Company’s Growth
Alisha Jerauld
Vice President of Environment, Social, and Governance
Affinity groups create spaces for networking, resources for mentorship, and training for professional development. Diverse workplaces enjoy improved financial success and growth, and data supports it. Studies suggest when efforts are made to curate a diverse workforce where all employees feel valued, regardless of gender, race, or other factors, it invites better innovation and boosts creativity—which leads to greater financial returns.
“Companies who have greater gender diversity on all levels of management outperform companies who don’t by as high as 25%,” says Alisha Jerauld, Vice President of Environment, Social, and Governance at Merit, referencing this 2020 study that followed the financial performance of companies who made efforts to be more inclusive. “When you have that type of diversity involved with strategizing, you have access to new ideas and perspectives, allowing the company to reach new markets and innovate new products.”
Building Bridges in STEM
Lucia Irazabal
Senior Engineer II
Vice Chair of WLI
As a leading medical device company, Merit offers a catalog of life-changing products that relies on the talented and creative engineers who design and build them. Lucia Irazabal, Senior Engineer II at Merit, became involved with the WLI in part to build a network of support for women in engineering and leadership positions to encourage employee retention.
“Both through my education and in the workplace, I have experienced being one of the few women on a team,” says Ms. Irazabal, vice chair of the WLI. “Merit is taking a great step developing the WLI. It’s important to have a space to share your perspective, find support, and relate to others who can offer both personal and professional guidance.”
Recently, the U.S. Census Bureau reported that even though women make up nearly half of the U.S. Workforce, only about 27% of STEM workers are women. As a result, women in STEM careers often discover it is more difficult to find a supportive network of those who share their experiences.
“Even the process of organizing the WLI has increased awareness of women in the workplace. I have had the opportunity to work with women from all areas of the company,” Ms. Irazabal says. As a testament to this observation, WLI meetings have been met with substantial interest with hundreds of employees, both men and women, voluntarily giving their time and attention to these important discussions.
Men Welcome, Too: Everyone Can Join the WLI
One of the chief goals of the WLI is to promote inclusion and share perspectives, and as a result, all employees are encouraged to join. Including everyone, regardless of gender, helps programs like the WLI thrive.
“Involving men helps them understand some of the challenges women and diverse employees face in the workplace,” Ms. Wood says. “Many of the men who joined told me they have women on their teams, and they want to be better prepared to help everyone succeed.”
While some of the barriers holding women back are big, others may go unnoticed until called into question. “When men are more aware of these issues, they often become allies who help to create positive change,” Ms. Jerauld says. “It helps by building a strong network of support.”
Looking Forward
The WLI is making positive strides at Merit, and Ms. Wood states there is more to come. “We plan to have one event each month over the next year that will focus on educating employees about a range of topics, from networking to career advancement,” she says.
The WLI believes by including and uplifting voices and perspectives, Merit will be better equipped to meet the goals outlined in the company mission:
UNDERSTAND. INNOVATE. DELIVER.
Let’s Talk Lung Cancer: An In-Depth Interview with Dr. Reddy

Lung cancer is the leading cause of cancer deaths worldwide.1 In the United States, more people die from lung cancer than any other type of cancer.2 November is Lung Cancer Awareness Month, and to help us gain a better understanding of the condition, the screening process, and treatment options, we sat down with Chakravarthy Reddy, MD, pulmonologist at the University of Utah Huntsman Cancer Institute in Salt Lake City, UT.
What Is Lung Cancer?
Lung cancer occurs when cells in the lungs change or mutate, resulting in abnormal cell growth. These cells multiply uncontrollably, forming a tumor and spreading to other parts of the body.
“Stage one or stage two, where patients are potentially curable, have almost no symptoms at all; it’s always incidentally found,” Dr. Reddy explains. “A patient has a scan for some other reason, and the cancer is detected in the lungs.”
When lung cancer symptoms do manifest, they can include a cough that worsens or does not resolve, chest pain, shortness of breath, coughing up blood, wheezing, weakness or fatigue, and weight loss.4 “Unfortunately, by the time a patient presents with symptoms, they’re in advanced stages, and their survival is not as good,” says Dr. Reddy.
What Are Risk Factors for Lung Cancer?
Smoking is by far the leading cause of lung cancer, putting people who smoke at a significantly higher risk of developing lung cancer compared to non-smokers.5
In addition to smoking, breathing secondhand smoke is also dangerous, increasing the risk of lung cancer.6 “We always talk about smokers, but there is a correlation between people who live with smokers and their risk for developing lung cancer,” Dr. Reddy adds. “Secondhand exposure does increase the risk of developing cancer.”
The American Cancer Society lists other risk factors for lung cancer, which include:5
Radon
A naturally occurring radioactive gas, radon is the breakdown of uranium in soil and rocks. Potential risk areas are homes with basements.
Asbestos
Asbestos is a mineral fiber that occurs in rock and soil.7 People who work with asbestos (e.g., in mines, mills, textile plants, shipyards, and where insulation is used) are several times more likely to die of lung cancer.
Carcinogens
Exposure to cancer-causing agents, such as uranium, arsenic, beryllium, cadmium, nickel compounds, coal products, and diesel exhaust can increase lung cancer risk.
Personal or Family History
If an individual has lung cancer, there is a higher risk of developing another lung cancer. Brothers, sisters, and children of people who have had lung cancer may have a higher risk.
Previous Radiation Therapy to the Lungs
People who have had radiation therapy to the chest for other cancers are at a higher risk of lung cancer, particularly if they smoke.
Air Pollution
In cities, air pollution can increase the risk of lung cancer, with some research suggesting approximately 5% of all deaths from lung cancer may be due to outdoor air pollution.
Who Should Be Screened for Lung Cancer?
The recommended screening test for lung cancer is a low-dose CT scan.8 According to the United States Preventive Services Task Force, those eligible for screening must meet the three-pronged criteria:9
Age ǀ Adults aged 50-80 years
Smoking History ǀ Individuals with a 20 pack-year smoking history
Tobacco Exposure ǀ Current smokers or those who have quit within the past 15 years
Age is a straightforward benchmark, but calculating a pack-year may seem foreign to most. “Multiply the number of packs of cigarettes you smoke per day by the number of years you’ve smoked. This gives you the value, which we call pack-years,” Dr. Reddy explains. An example would be if a person has smoked a pack of cigarettes for 20 years or two packs for 10 years, each of these instances would calculate a 20 pack-year history.
The third criterion addresses tobacco exposure—but what is the significance of a 15-year time span? “It takes about 15 years for the risk [of lung cancer] to normalize,” Dr. Reddy says. “If it’s been less than 15 years since the patient quit, then the third criterion for lung cancer screening is met.”
This also means if a patient does not meet the criteria, screening will not happen. Dr. Reddy encourages people who are under 50 who have a 20 pack-year history to speak with a physician about any concerns, personal risk factors, and the benefits of being screened.
What Lung Cancer Treatment Options Are Available?
When lung cancer is caught early, there are more curative options. Unfortunately, as Dr. Reddy mentioned, lung cancer is normally caught in late stages. A surgery called a lobectomy, which removes one of the lobes in the lung, is only an option for stage 1 or 2 cancer. “Patients who come in with lung cancer don’t have healthy lungs to begin with,” Dr. Reddy says. “It’s more likely they also have emphysema from smoking, and they probably won’t tolerate removal of even a lobe.”
If a patient’s lung function is borderline, Dr. Reddy suggests another surgical option called a wedge resection, where the lobe is spared, and only the cancer is removed. “It’s not preferred, but if that’s the only option, it’s better than not doing anything,” Dr. Reddy says. “If their lung function is any worse than that, then we clearly cannot do any surgery at all. We have to think of second-line approaches, such as radiation therapy.”
According to Dr. Reddy, lung cancer that spreads first to the lymph nodes in the chest is still potentially curable. However, once it leaves the chest and invades the chest cavity and other parts of the body, such as the adrenal glands, the brain, or bones, it is potentially no longer curable. When this occurs, palliative care is the only option, relieving symptoms and mitigating suffering while optimizing patient quality of life.
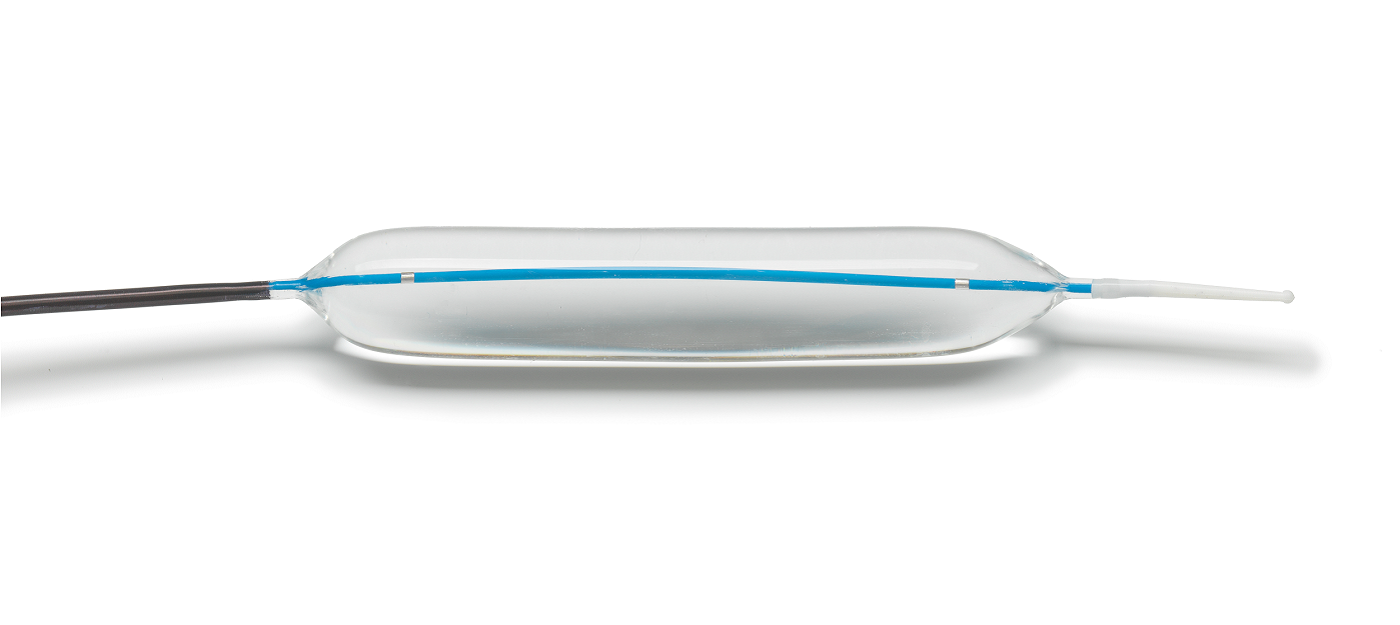
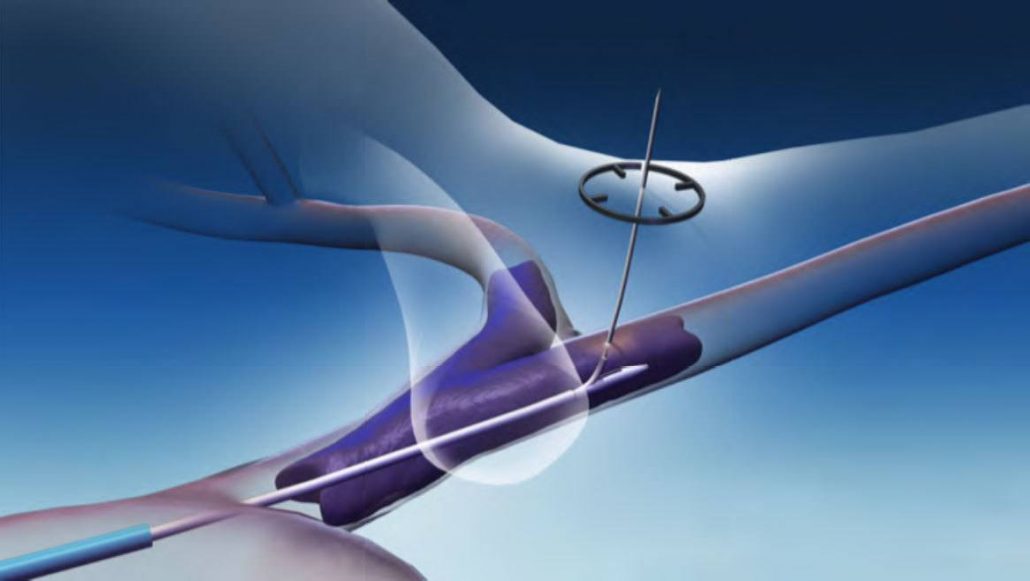
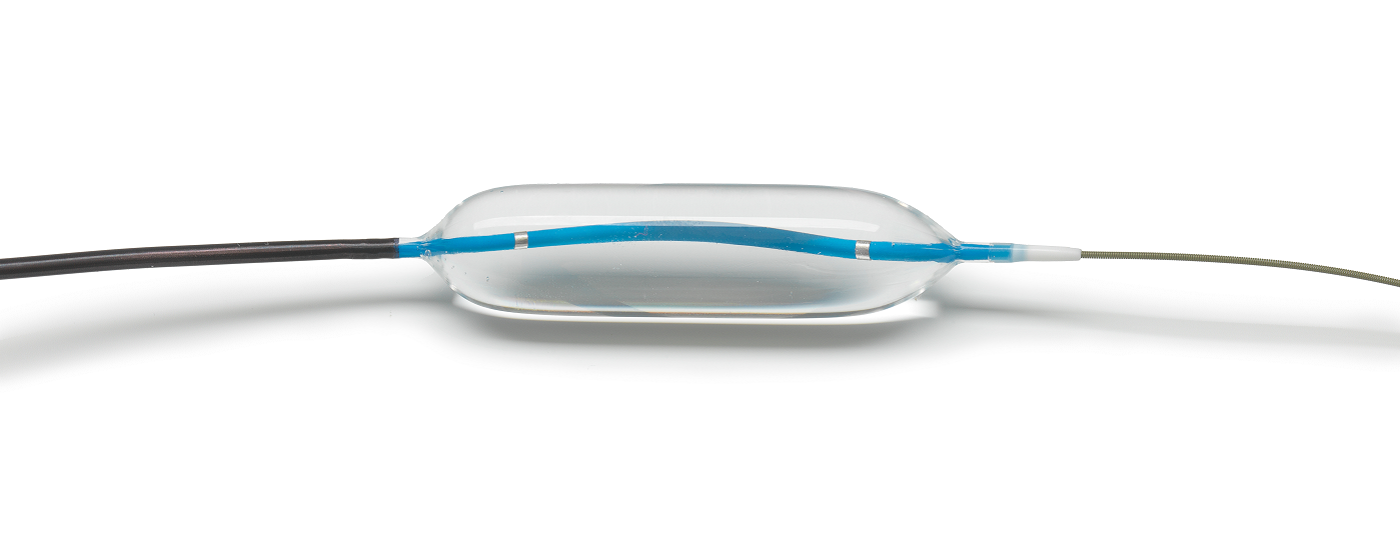
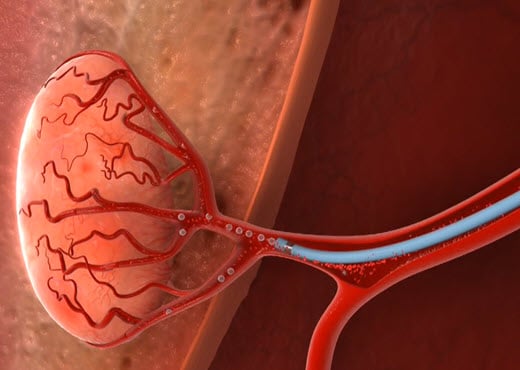
To relieve common lung cancer symptoms, such as shortness of breath or a persistent cough, there are options. “One of the things we do is use balloons to dilate [the airway passages],” Dr. Reddy explains. “Merit makes Elation® balloons, which we find extremely useful, especially because they are available in short, two-centimeter balloon configurations.”
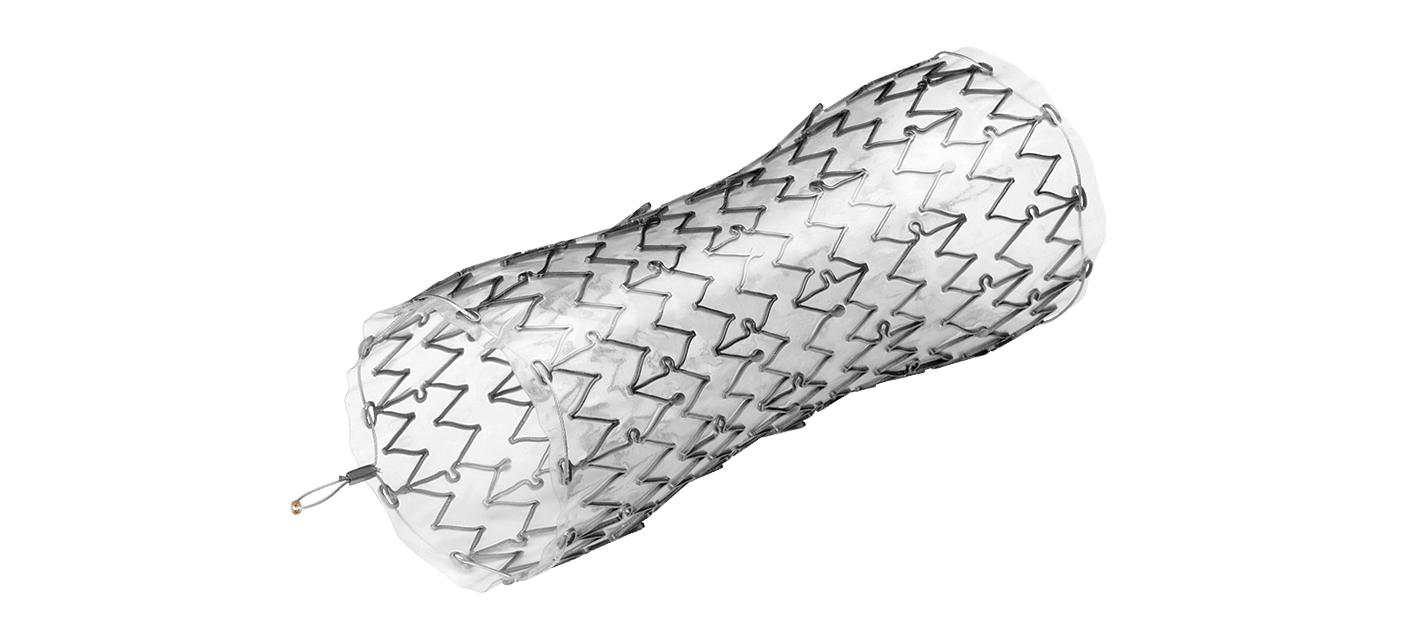
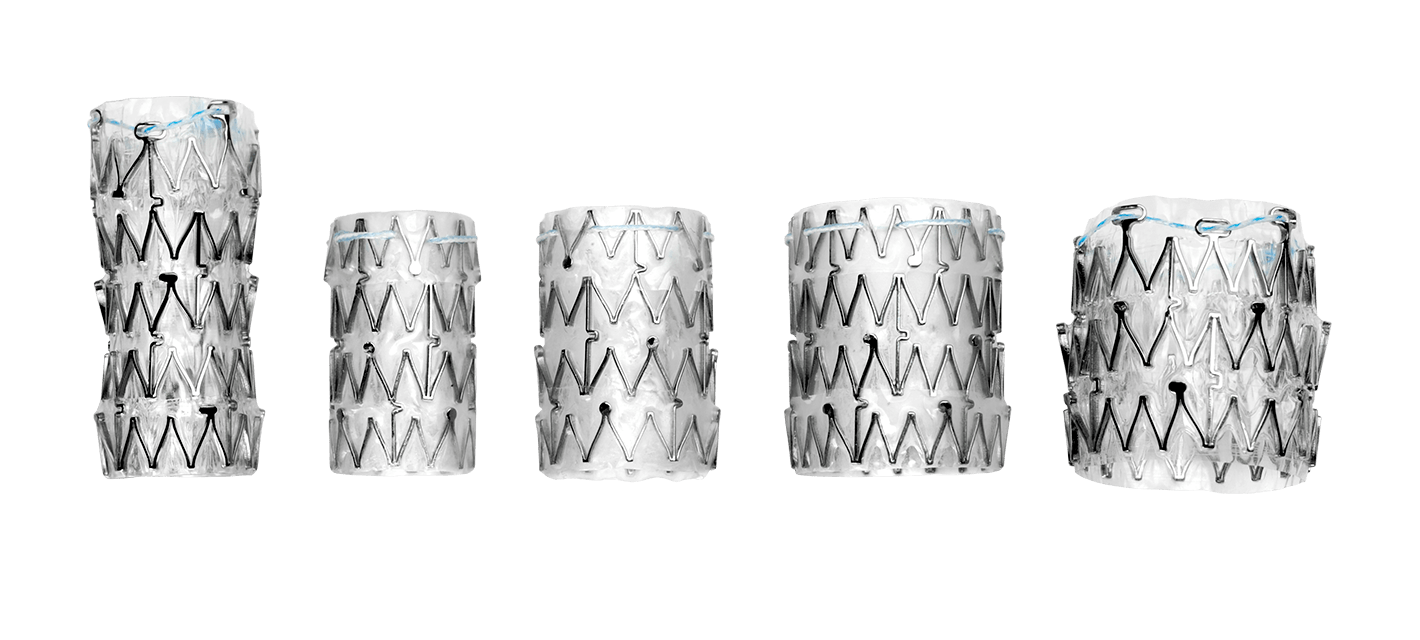
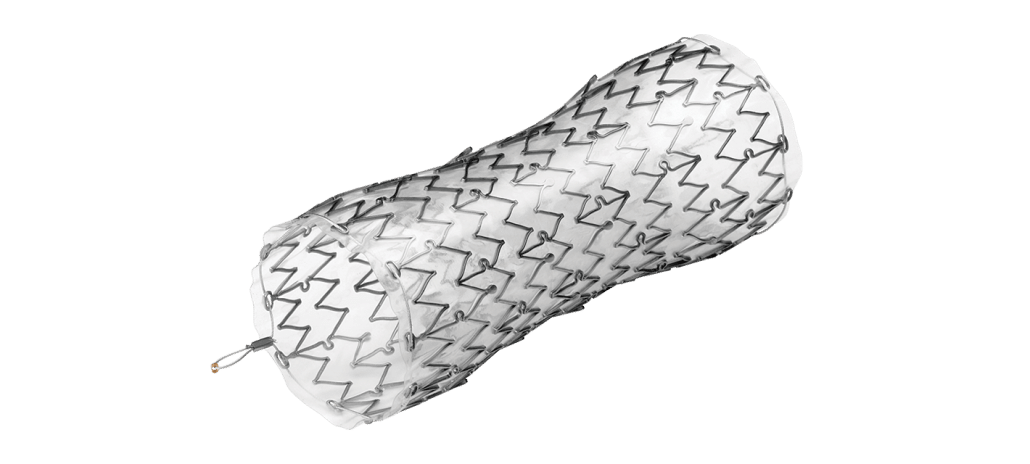
A second approach is to stent the tumor in the lung to maintain the patency of the airway. An option for this line of treatment would be Merit’s AERO® Tracheobronchial Stents. “Patients notice an improvement immediately, almost right after they wake up from the procedure,” Dr. Reddy says. “The radial force of the AERO stent actually keeps the airway open, and that improves shortness of breath.”
Lung Cancer Awareness Resources
As lung cancer awareness is heightened this month, it is critical to share facts about the importance of screening with loved ones and encourage those who smoke to quit.
Knowledge is power, and having health resources to help understand lung cancer better is important. In addition to information about the disease, the below organizations provide a wide range of topics, including survivor stories and ways to get involved throughout the month, helping patients and families in their battle against lung cancer:
Lung Cancer Foundation of America
American Lung Association
GO2 Foundation for Lung Cancer
Support for Merit Employees
If you smoke and need help quitting, sign up for our Employee Smoking Cessation program. Contact Dr. Priest for more information.
Merit Medical is dedicated to improving the lives of people, families, and communities worldwide. Learn more about the trusted interventional and palliative treatment options we offer to help physicians care for lung cancer patients.
References:
- World Health Organization. 2021. “Cancer Key Facts.” https://www.who.int/news-room/fact-sheets/detail/cancer
- Centers for Disease Control and Prevention. 2021. “Lung Cancer Statistics.” https://www.cdc.gov/cancer/lung/statistics/
- American Lung Association. 2021. “Lung Cancer Basics.” https://www.lung.org/lung-health-diseases/lung-disease-lookup/lung-cancer/basics
- Centers for Disease Control and Prevention. 2021. “What Are the Symptoms of Lung Cancer?” https://www.cdc.gov/cancer/lung/basic_info/symptoms.htm
- American Cancer Society. 2019. “Lung Cancer Risk Factors.” https://www.cancer.org/cancer/lung-cancer/causes-risks-prevention/risk-factors.html
- Centers for Disease Control and Prevention. 2021. “Health Effects of Secondhand Smoke.” https://www.cdc.gov/tobacco/data_statistics/fact_sheets/secondhand_smoke/health_effects/index.htm
- United States Environmental Protection Agency. n.d. “Learn About Asbestos.” https://www.epa.gov/asbestos/learn-about-asbestos
- Centers for Disease Control and Prevention. 2021. “Who Should Be Screened for Lung Cancer?” https://www.cdc.gov/cancer/lung/basic_info/screening.htm
- United States Preventive Task Force. 2021. “Lung Cancer: Screening.” https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/lung-cancer-screening
Merit’s Commitment to Breast Cancer Awareness

Throughout October, Merit joins Breastcancer.org to advocate the importance of mammography screening in detecting breast cancer at its earliest stages.
For those diagnosed with breast cancer and undergoing surgery, watch the video below to see how SCOUT® is improving the patient experience.
Want to see how Merit employees were supporting Breast Cancer Awareness in 2021? Take a look here.
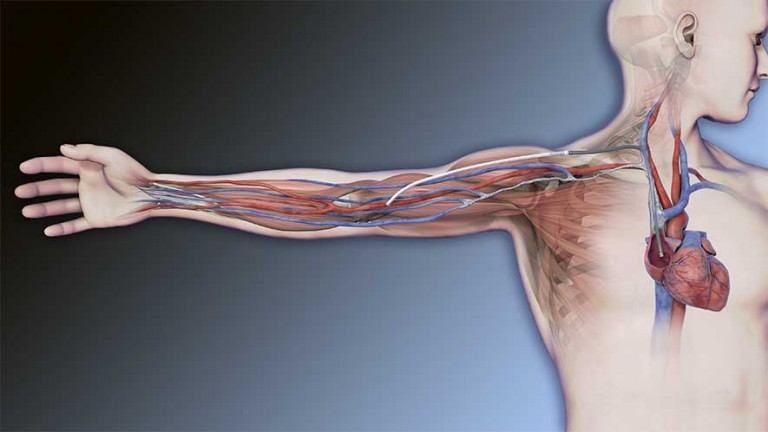
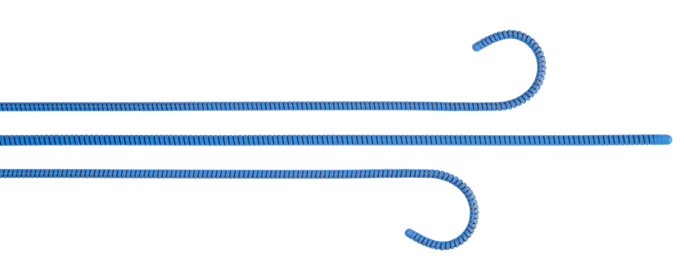
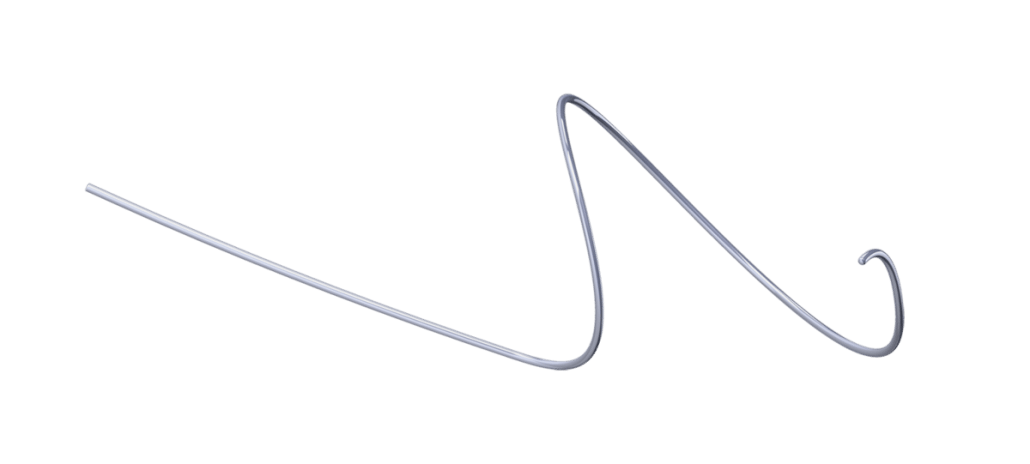
ClariVein® OC 5-Year Follow-up Results: Good Occlusion Rate, No Major Complications
Chronic venous insufficiency (CVI) in the legs, also known as varicose veins, is a relatively common condition, with worldwide prevalence ranging between 10% and 30%. Varicose veins can result in a number of symptoms, including pain, leg swelling, itching, and skin discoloration. Individuals with the condition may experience diminished quality of life and loss of work productivity. Finding treatment options that are effective and comfortable for the patient have been an area of interest in the endovascular community.
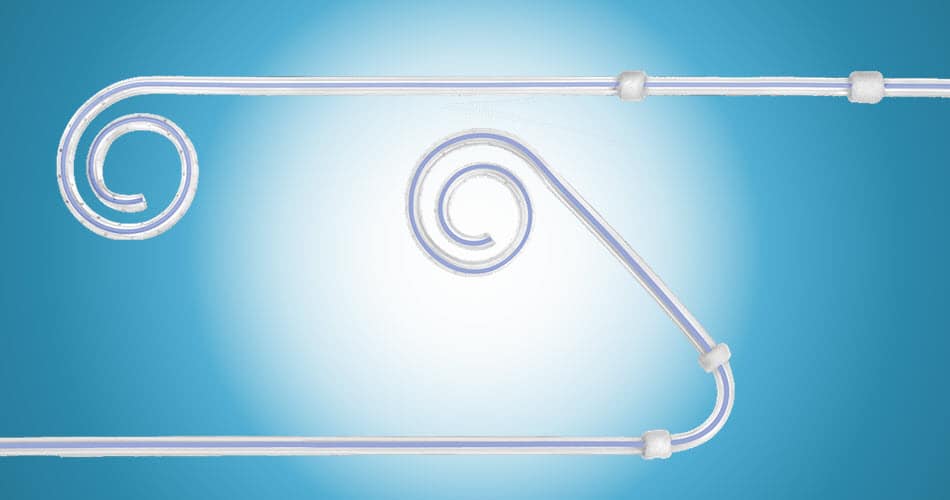
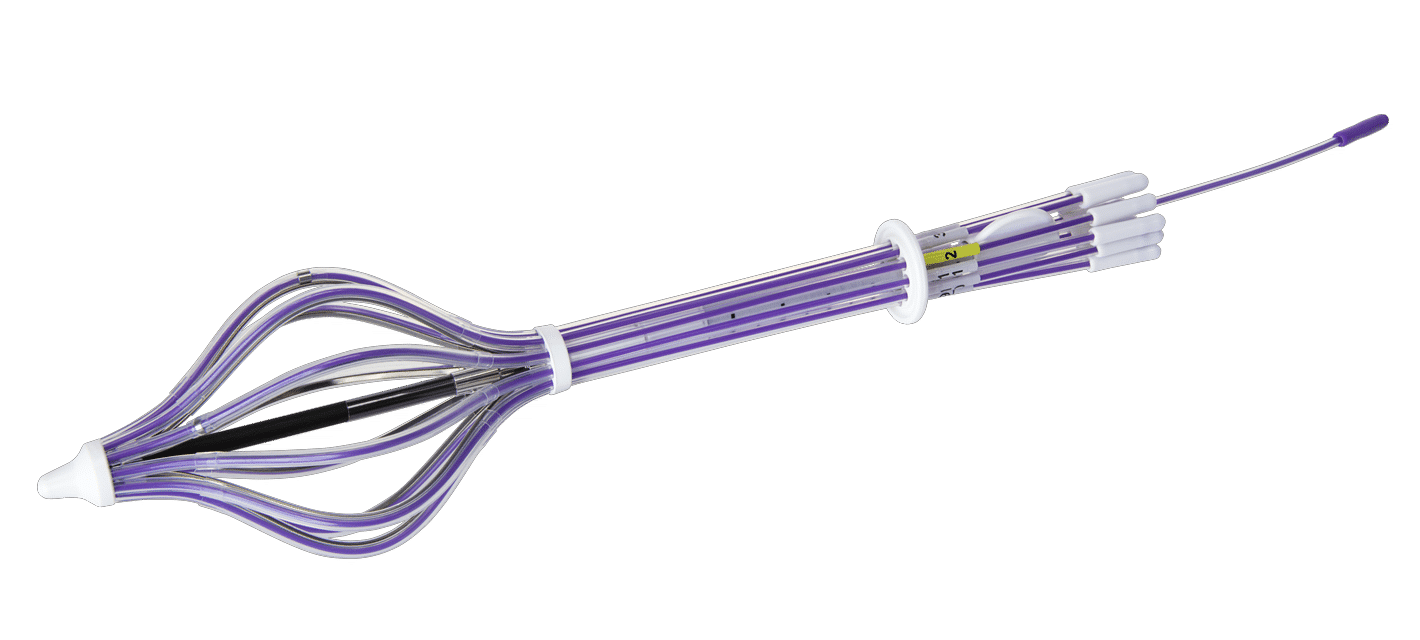
A study by researchers in Verona, Italy, found that endovenous mechanochemical ablation (MOCA) treatment with the ClariVein® OC Infusion Catheter was associated with a good occlusion rate, comparable with other techniques, including thermal techniques, without major complications. This is one of the first reports in literature for MOCA treatment of symptomatic varicose veins with 5-year results. With little long-term data pertaining to this type of treatment, the aim of the study was to evaluate long-term occlusion rates.
This retrospective single-center study was published in Journal of Vascular Surgery: Venous and Lymphatic Disorders. Mirandola et al. treated 395 primary, symptomatic, unilateral, incompetent varicose saphenous veins in an outpatient setting. Of these patients, none were treated bilaterally in the same session. The majority of vessels treated were great saphenous veins (92.3%), and the others were small saphenous veins. Procedures were performed with the ClariVein OC and polidocanol 2% in liquid form.

The overall survival rate free from recanalization was 92.4%. Anatomic success was 94% at 1 year, 91% at 2 years, 88% at 3 years, 88% at 4 years, and 84% at 5 years. The follow up at 5 years included 23 patients, five of whom presented with recanalization. The authors note that in this series, the veins completely disappeared on duplex ultrasound scan in 36% of cases.
It is interesting to note that after 89 patients, the researchers changed the way in which the sclerosant was injected. Beginning the infusion of sclerosant at point of mechanical pullback (protocol 2) produced higher occlusion rates compared to traditional ClariVein OC technique (protocol 1) with delayed infusion of sclerosant. Protocol 2 resulted in a change in cumulative survival rate free from recanalization from 92% to 97% (P = 0.013).
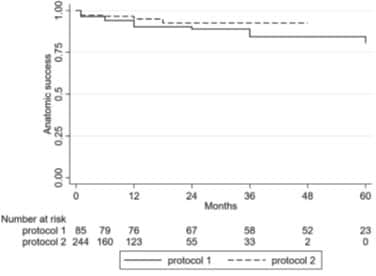
The researchers concluded that the ClariVein OC was associated with a good occlusion rate and was comparable with other techniques, including thermal techniques, without major complications.
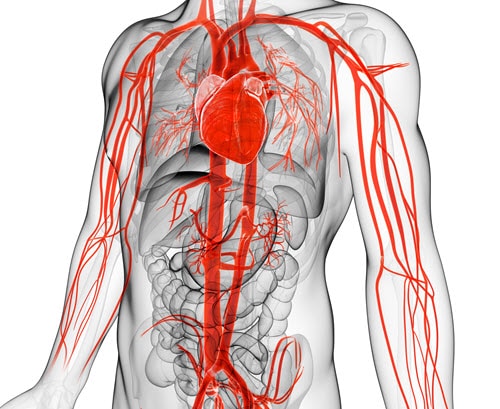
Varicose veins occur when vessels are unable to pump blood back to the heart, causing the blood to pool, resulting in vessel enlargement over time. Under normal conditions, blood moves from the heart to the legs through the arteries and back to the heart through the veins. To accomplish this, the veins rely on surrounding muscles and a collection of valves to prevent blood from flowing backward. When these muscles and valves weaken or fail to work, blood begins to gather in the vein instead of returning to the heart.
In addition to pain, swelling, itching, and skin discoloration, other symptoms of varicose veins include:
- Twisted and bulging veins
- Aching, burning, throbbing and muscle cramping
- Leg heaviness and fatigue
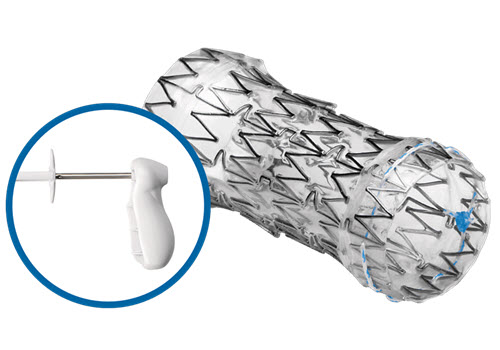
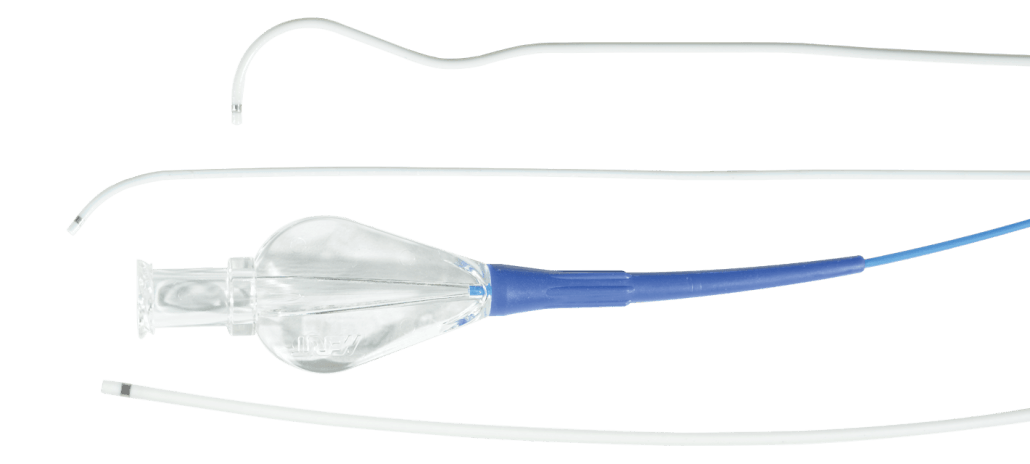
The ClariVein OC alleviates these symptoms by combining the power of a specialty infusion catheter with a rotating wire tip designed for the controlled 360-degree dispersion of physician-specified agents inside the targeted vessel. Requiring only a pin-sized entry through the skin, treatment with the ClariVein OC takes very little time, uses no heat or tumescent anesthesia, and creates minimal discomfort to the patient.
Learn more about the clinically proven ClariVein OC and how it can change the lives of your patients. Visit ClariVein.com or contact our Customer Support for more information.
ARTICLE REFERENCED:
Mirandola M et al. 2020. “An Italian Experience with Mechanochemical Ablation of the Saphenous Vein Since 2012.” J Vasc Surg Venous Lymphat Disord 8, no 6 (Nov): 999–1005. PMID: 32179039.
Meet the One-Vac™, Merit’s Newest Evacuated Drainage Bottle

The One-Vac is a valued addition to Merit’s Drainage portfolio and accompanies other premier products, such as the Aspira® Drainage System. This extension of the Drainage portfolio is the result of Merit’s commitment to continued innovation and dedication to providing clinicians with multiple high-quality product options when treating patients.
Several key features are designed to make the One-Vac easy to use, helping to reduce the occurrence of common issues associated with bottle use.
KEY FEATURES & BENEFITS
1 – Ergonomic Handle
Start, stop, and regulate flow. Easy to remove, minimizing spills during discard.
2 – Easy Sampling
Connect syringe and open handle to remove fluid for sampling.
3 – Bottle Neck
Easy to hold.
4 – Durable Plastic
Designed to prevent breakage.
5 – Faster Flow Rates
Provides 68% faster flow rates than competitive evacuated bottles.1
Learn more about the One-Vac Evacuated Drainage Bottle by exploring its product page or by connecting with our Customer Support Center to see how you can incorporate it and other Merit solutions into your practice today.
REFERENCES
1. Data on file.
A Physician’s Perspective on Wire-Free Localization

INTRODUCTION
Everett Bonner, MD, is a general surgeon specializing in surgical breast oncology at the Baton Rouge Clinic a large, multi-specialty clinic in Baton Rouge, LA. Dr. Bonner joined the group after completing his Surgical Breast Oncology Fellowship at Memorial Sloan-Kettering Cancer Center, New York, NY.
Dr. Bonner performs on average 25-30 breast surgical procedures a month at Baton Rouge General Hospital, which implemented their wire-free program with SCOUT in 2019. Dr. Bonner led the SCOUT implementation and shares his perspectives.
What was your primary motivator in evaluating and switching to a wire-free technology?
I think the biggest motivating factor was the problems we had with wire localization. Let’s be honest, no one likes them, not the physicians and certainly not the patients. Wires were becoming dislodged; patients were a bit “freaked out” about a 10-inch wire hanging out of their breast covered by a paper cup.
I always thought sterilization was an issue. We are always so conscious of this in the OR, yet we have this 10-inch wire that was exposed to all kinds of elements for a few hours. I say that a localization with SCOUT facilitates a more sterile surgery.
I also perform Hidden Scar Surgery, and a wire localization made it very difficult for me to place the incision exactly where I wanted. Utilizing the SCOUT technology has eliminated that issue. I have total freedom to place my incision where the patient will not see it and have a constant reminder of her cancer. In a lot of my cases, I can make one hidden incision under the arm for the tumor and the sentinel node.
It has revolutionized my practice – it has been a game changer.
Were you familiar with other wire-free technologies?

We did not trial SCOUT first. We trialed two other wire-free options, and we were not very happy. With one we had to continuously adjust equipment, and with the other we would have needed to switch to a whole new standard of surgical instruments.
For us, SCOUT was the technology of choice. It was more user friendly, and we would not have to rebuy all new instrumentation. It has worked out extremely well for the hospital, for our practice, and we have never looked back. In fact, my associates and I now almost localize exclusively with SCOUT, and most of us have not used a wire localization in more than a year.
Since using SCOUT, how has it affected your surgical outcomes?
It has been a game changer in three key areas. First and foremost, my re-excision rate is down to less than 5% (the national average is about 10%). I spend less time in the OR, and infection rates have dropped.
I think a very important point is that I use SCOUT, not only for localization, but for real-time guidance during surgery. I am constantly using SCOUT as I am doing my circumferential dissection around the tumor. I am constantly relocating to make sure I am not too close to the tumor, and once I have removed the tumor, I do a margin assessment circumferentially. If it looks like I am too close into a particular margin, I will go back and take additional tissue.
Also, not to be minimized is the fact that I can perform a lumpectomy in about 30 – 45 minutes, as opposed to the hour and a half it normally takes with a wire localization. That is less OR time, less anesthesia for the patient, which all adds up to safety and cost savings.
What can you tell us from a patient’s perspective about a wire-free experience?
Patients love it! I do a lot of patient education upfront, and I am very detailed in explaining the whole surgical experience. I get rave reviews on how “cool” SCOUT, is and they love that they cannot see or feel it, especially patients who have had a past wire localization experience.
At first, I did get a bit of push back about making a trip to the hospital to get the reflector placed, but once I explain that it can be done in conjunction with pre-admission testing, that concern was alleviated.
Patients really appreciate the value of new technology. It is good for them and good for the practice. Being on the forefront of new technology has improved my patient volume. We do little advertising. Therefore, its popularity has been purely by word of mouth.
What are the main outcomes a physician should expect from their wire-free technology?
The number one thing is cleaner margins and the potential to decrease your re-excision rate. Like I mentioned before, my rate is now half of what it was with a wire.
Number two is patient comfort and satisfaction. Patients are nervous enough going to surgery. Add the discomfort and the trauma of a wire sticking out of their breast and that is not patient centric. SCOUT has changed all of that.
The third one, and I think also a major consideration, is precision. You can take less tissue because you know exactly where you are going as you dissect the tumor, which results in a more cosmetically appealing result. Some surgeons say, “Just take a larger tissue sample.” But my question is why when SCOUT is so precise? With this localization and guidance technology, you can take less tissue and have good margins as well as a better cosmetic outcome.
Continuing Education: Why It’s Vital to Improving Patient Care
Think Education™ proctors discuss the purpose continuing education serves in an evolving medical industry and how the Think Education program is paving the way for better learning opportunities now and into the future.


“Physician education allows us to remain at the forefront of knowledge,” says Darren Klass, MD, PhD, MRCS, FRCR, FRCPC, Think Radial® Proctor. “It has a dramatic impact on patient care in that it allows physicians to provide the latest treatment. In many instances, the procedure itself may not fundamentally change; however, new techniques and equipment that make the procedure safer and more effective can improve patient outcomes.”
Not only does continuing education keep physicians informed, it also helps to ensure patients are, too. Being aware of all treatment options can mean the difference between undergoing a minimally invasive procedure or conventional surgery. Utilizing less invasive techniques can minimize risk to the patient, reduce pain as well as recovery time in comparison to open surgery. 2
“Even if physicians are not bringing new skills and developments directly into their own working environment, the awareness of new alternatives is valuable,” explains Ferdinand Kiemeneij, MD, PhD, Think Radial Proctor. “Patients will benefit by either receiving state-of-the-art treatment, or they are at least aware of alternatives if the physician involved informs them properly.”
Program topics include interventional techniques for airway stenting, the implantation of LV leads, and minimally invasive treatment of pathologic vertebral fractures and metastatic spinal tumors. Other course topics include embolization for the treatment of symptomatic benign prostatic hyperplasia, peritoneal dialysis implantation, radial and distal access, and wire-free tumor localization. Explore Merit’s courses here.
Designed and taught by physicians, each course immerses attendees in a number of ways, including didactic presentations, taped or live cases, and state-of-the-art, hands-on training. Encompassing all aspects of a procedure or disease state, Think Education courses provide physicians with the up-to-date knowledge they need to immediately put what they learn into practice. Both virtual and on-demand courses are available.
“The courses evolve each time they are presented in order to provide physicians with the latest data and experience, presented in an unbiased way that is first and foremost about improving patient care,” Dr. Klass says. “Probably the biggest impact the Think courses have is their clear message of intercollegiate collaboration. Physicians are able to listen to experts speak on their respective fields—which is unique to the Think Education program.”
“Think Education is an invaluable asset to the medical community,” explains Brett Parkinson, MD, Think Wire-Free™ Proctor. “It provides opportunities for physicians to learn in a friendly, relaxed environment, and because course topics involve cutting-edge technology, attendees come away knowing they have added the latest treatment options to their armamentarium of care.”
“As a proctor for Think Education programs, I believe physician-to-physician interaction gives attendees confidence that they are getting experienced thought leaders in their field,” says Michael Hallisey, MD, Think Spine™ Proctor. “This gives them the chance to expand their knowledge and improve their medical practice.”
As continuing education adapts to the changing needs of physicians, it brings with it the opportunity to influence and improve future opportunities to learn, serving as a catalyst for better programs that have a broader reach.
“Physician education will continue to expand in the online format in the future. This can allow top physicians to share their expertise with a larger part of the world,” Dr. Hallisey says. “We all want more confidence and skill in treating patients. A well-educated physician can have that.”
Learn more about Merit’s Think Education program and sign up for an upcoming course today.
REFERENCES
1. American Association of Continuing Medical Education. 2020. “Importance of CME.” https://aacmet.org/cme/importance-of-cme/
2. Johns Hopkins Medicine. 2021. “What Is Vascular and Interventional Radiology?” https://www.hopkinsmedicine.org/interventional-radiology/what_is_IR.html
3. Chirag V et al. 2020. “Socially Distant Medical Education in the Face of COVID-19.” Med Sci Educ Oct 21: 1–3. PMID: 33106763
Embosphere® Results in Less Inflammatory Response, Lower Rates of Analgesic Use Compared to PVA After UFE
Every July, our team at Merit Medical recognizes Fibroid Awareness Month as a time to bring attention to a very common yet under-discussed condition that will affect most women at some point in their lifetime.
We do this by supporting a minimally invasive fibroid treatment called uterine fibroid embolization (UFE), also called uterine artery embolization (UAE), through a portfolio of embolotherapy products we offer.
Published in Radiology, the study enrolled 54 women with fibroids (mean age, 44 ± 4 years [standard deviation]) and assigned UFE treatment with either nonspherical PVA (355–550 μm) or Embosphere (500–700 μm). There were 27 women in each group, and both participants and investigators collecting data were blinded to the embolic material used. Women with concomitant disease (e.g., adenomyosis) were excluded from the study.
Both groups were given fentanyl-based intravenous patient-controlled analgesia within the first 24 hours after UFE as well as rescue analgesics. The investigators measured neutrophil-to-lymphocyte ratio to assess inflammatory response, and contrast-enhanced MRI was performed 1 day after the procedure to evaluate dominant fibroid necrosis and ischemia of normal myometrium. Symptom severity score and health-related quality-of-life score were assessed before and 3 months after UFE.
Results showed that pain scores and fentanyl dose were not different during the first 24 hours, but the use of rescue analgesics was higher in the PVA group (33% vs 11%; P = 0.049). After embolization, symptom severity score and health-related quality-of-life score were not different between groups (symptom severity score: 16 [interquartile range, 6–22] for PVA vs 19 [interquartile range, 9–34] for Embosphere, P = .45; health-related quality-of-life score: 93 [interquartile range, 80–97] for PVA vs 89 [interquartile range, 84–96] for Embosphere, P = .41).
In addition, changes in neutrophil-to-lymphocyte ratio from before to 24 hours after UFE were greater in the PVA group (3.9 [interquartile range, 2.7–6.8] compared to the Embosphere group (2.5 [interquartile range, 1.5–4.6]; P = .02). Rates of complete dominant fibroid necrosis were not different between groups, but transient global uterine ischemia of normal myometrium was more frequent in the PVA group (44% vs 15%; P = .04).
The investigators of the study concluded that when used in UFE, PVA particles and Embosphere resulted in similar pain scores and fentanyl dose. However, PVA resulted in a greater inflammatory response, higher rates of rescue analgesic use, and more frequent transient global uterine ischemia compared to Embosphere.
Watch How UFE Works
Fibroids (also known as uterine fibroids, leiomyomas, and myomas) are non-cancerous tumors that grow within the muscle tissue of the uterus. Although some fibroids cause no symptoms at all, common symptoms can include excessive menstrual bleeding, pelvic pain and pressure, and frequent urination. Depending on the size and location of the fibroids, other symptoms can include anemia, leg pain, pain during sexual intercourse, constipation, and an enlarged abdomen. Up to 80% of women develop fibroids by the time they reach age 50.
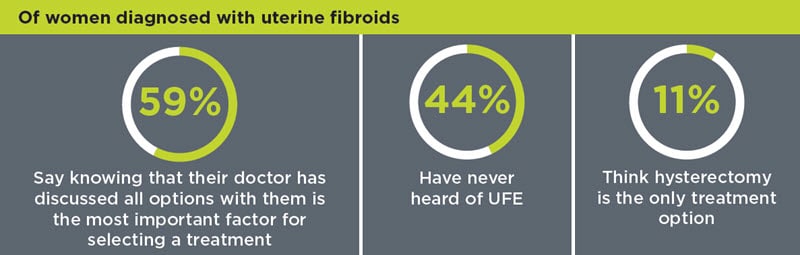
Approximately, 600,000 hysterectomies are performed in the US each year, with fibroids listed as the most common reason. A report by the Society of Interventional Radiology found that 1 in 5 women believe hysterectomy is the only treatment option for fibroids and that 44% of women with fibroids have never heard of UFE. Although hysterectomy is a treatment for fibroids, there are many other treatment options available, many of which are minimally invasive.
To encourage women to seek out all treatment options and help physicians educate patients, we offer an educational patient-awareness site called Ask4UFE with information about treatment options—with focus on UFE—as well as patient and physician testimonials and researched blog entries.
Join us in recognizing July as Fibroid Awareness Month. We look forward to working together to increase awareness surrounding the condition, helping to provide the best resources, products, and care for patients worldwide.
Before using, refer to Instructions for Use (IFU) for indications, contraindications, warnings, precautions, and directions for use.
ARTICLE REFERENCE
Han K et al. 2020. “Nonspherical Polyvinyl Alcohol Particles verusus Tris-Acryl Microspheres.” Radiology 298, no. 2 (Feb): 458–465. PMID: 33350893.
Merit Brings Awareness to Men’s Health During the Month of June

At Merit Medical, it’s our goal to not only provide the tools physicians need to treat and improve patient outcomes but also share knowledge and increase awareness surrounding risk factors for disease.
We understand that illness affects both men and women, but to offer the best patient care, it’s also important to shed light on diseases that are more prevalent in one sex versus the other.
Here are just some of the illnesses that are seen more frequently among men—and how we help care for each.
ESOPHAGEAL CANCER
Esophageal cancer is cancer found in the esophagus—the hollow, muscular tube in your body that carries food and liquid from the throat to the stomach. Men are around three times more likely than women to have esophageal cancer.
- Avoid alcohol.
- Eat more fruits and vegetables.
- Maintain a healthy weight.
- Exercise regularly.
Learn more about esophageal cancer.
MERIT PRODUCTS
LUNG CANCER
Lung cancer is a type of cancer that begins in the lungs. It is the leading cause of cancer deaths worldwide. The overall chance of a man developing lung cancer in his lifetime is approximately 1 in 15, whereas for a woman, the risk is about 1 in 17.
- Quit smoking (or don’t start).
- Stay away from secondhand smoke.
- Test your home for radon.
- Avoid cancer-causing chemicals.
- Live a healthy lifestyle.
MERIT PRODUCTS
KIDNEY FAILURE
Although more women than men are diagnosed with chronic kidney disease, or CKD, men are more likely to reach kidney failure sooner.
Although kidney failure can happen to anyone, men may be more at risk compared to women due to differences in hormones and living unhealthier lifestyles.
- Get a kidney check-up at least every year.
- Control your blood pressure and blood sugar.
- Stop smoking (or don’t start).
- Exercise and eat a healthy diet.
- Maintain a healthy weight.
- If you have an enlarged prostate, talk with your doctor to make sure it’s not blocking your urinary tract.
- Give your doctor a list of any supplements, medicines, and/or hormone treatments you’re taking to ensure they aren’t damaging your kidneys.
Learn more about kidney failure and visit our Dialysis Access Solution page.
MERIT PRODUCTS
AORTIC ANEURYSM
The aorta runs from the heart through the center of the chest and abdomen. It’s the main blood vessel that brings blood to the abdomen, pelvis, and legs. An abdominal aortic aneurysm (AAA) is a life-threatening condition that occurs when the vessel enlarges, putting it at risk of bursting. Men are 4-15 times more likely to develop an AAA than women
- Stop smoking (or don’t start).
- Reduce stress.
- Exercise and eat a heart-healthy diet.
- If you have diabetes or high blood pressure, take the medicines your doctor has prescribed.
Learn more about AAA. To learn more about our packs, wires, and other cardiac products, please visit our Merit Vascular page.
MERIT PRODUCTS
HEART ATTACK
A heart attack, also known as a myocardial infarction, occurs when heart muscle doesn’t receive enough blood. As time passes without receiving treatment, the more damage is done to the heart. The main cause of a heart attack is coronary artery disease (CAD). Researchers have found that throughout life, men are about twice as likely as women to have a heart attack.
- Eat a healthy diet.
- Maintain a healthy weight.
- Exercise regularly.
- Stop smoking (or don’t start).
- Monitor your cholesterol and blood pressure.
- Manage your diabetes.
- Take your prescribed medicines.
Learn more about heart attacks. Explore our Cardiac Portfolio, including our radial sheaths, catheters, wires, and compression devices.
MERIT PRODUCTS
LIVER CANCER
Hepatocellular carcinoma (HCC) is the most common type of primary liver cancer and is most often seen in people with chronic liver diseases, such as cirrhosis caused by hepatitis B or hepatitis C. Worldwide, HCC is the fourth leading cause of cancer death and is 3 times more common among males than females.
- Avoid heavy alcohol use.
- Reduce exposure to aflatoxin B1.
- Stop smoking (or don’t start).
- Get the hepatitis B vaccine.
- If you have hepatitis, work with your care provider to receive treatment.
Learn more about liver cancer. Visit our Hepatic Oncology portfolio.
MERIT PRODUCTS
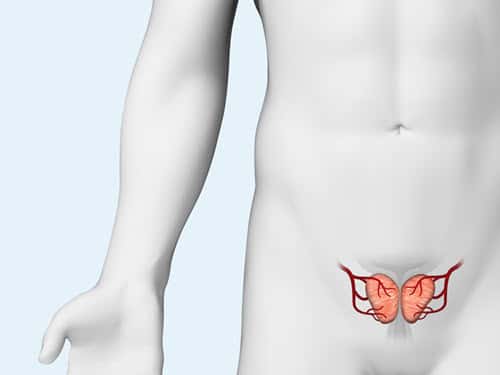
BENIGN PROSTATIC HYPERPLASIA (BPH)
Benign prostatic hyperplasia, or BPH, is the enlargement of the prostate gland and affects only men. It becomes more common as men get older. Up to 90% of men over the age of 80 have BPH. Although BPH is noncancerous, it can cause bothersome lower urinary tract symptoms.
- Maintain a heart-healthy diet.
- Avoid heavy alcohol use.
- Exercise regularly.
Explore the products we offer to support prostatic artery embolization (PAE), a minimally invasive option to treat BPH.
MERIT PRODUCTS
At Merit Medical, our goal is to improve the lives of people, families, and communities worldwide. An important part of this is caring for men’s health by providing the products and therapies needed for patients to live at their best.
Have questions? Reach out to our Customer Support team.
Before using, refer to Instructions for Use for indications, contraindications, warnings, precautions, and directions for use.
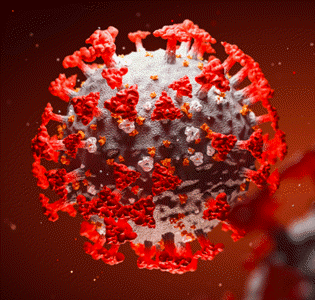
Merit Medical Leads Wire-Free Localization as SCOUT® Procedures Surpass 200,000
Merit Medical has achieved an important milestone as SCOUT surpassed 200,000 procedures—far exceeding any other non-radioactive wire-free device. Launched in 2016, SCOUT has realized remarkable growth and system-wide adoption in the US and global expansion since 2020. Our commitment to ongoing product enhancements, customer training and support, and clinical education contributes to this achievement. However, this milestone would not be possible without the input and support of our valued customers.

HOW DID WE GET HERE? THE SCOUT PLATFORM
With clinically insignificant MRI artifact, there is no restriction on the imaging modalities that can be used effectively throughout a patient’s treatment. This gives physicians the ability to place a reflector at the time of biopsy, prior to neoadjuvant chemotherapy (NAC), and to enable targeted axillary dissection. While SCOUT has been used primarily for breast tumor localization, physicians are recognizing the clinical benefits, including 1+/- mm accuracy, 60-mm depth, and 360° detection, are applicable for myriad oncological applications, including nodes, sarcoma, and lung.
1+/-
mm
Accuracy
60 mm
Depth
360°
Detection
OUR COMMITMENT TO YOU
Merit Medical remains committed to you, your staff, and the patients you serve. We are dedicated to delivering exceptional customer service as well as more product enhancements and platform expansion to help reduce the burden cancer places on your patients and their loved ones. Thank you for your ongoing support and partnership through our journey to market leadership in wire-free localization with SCOUT.
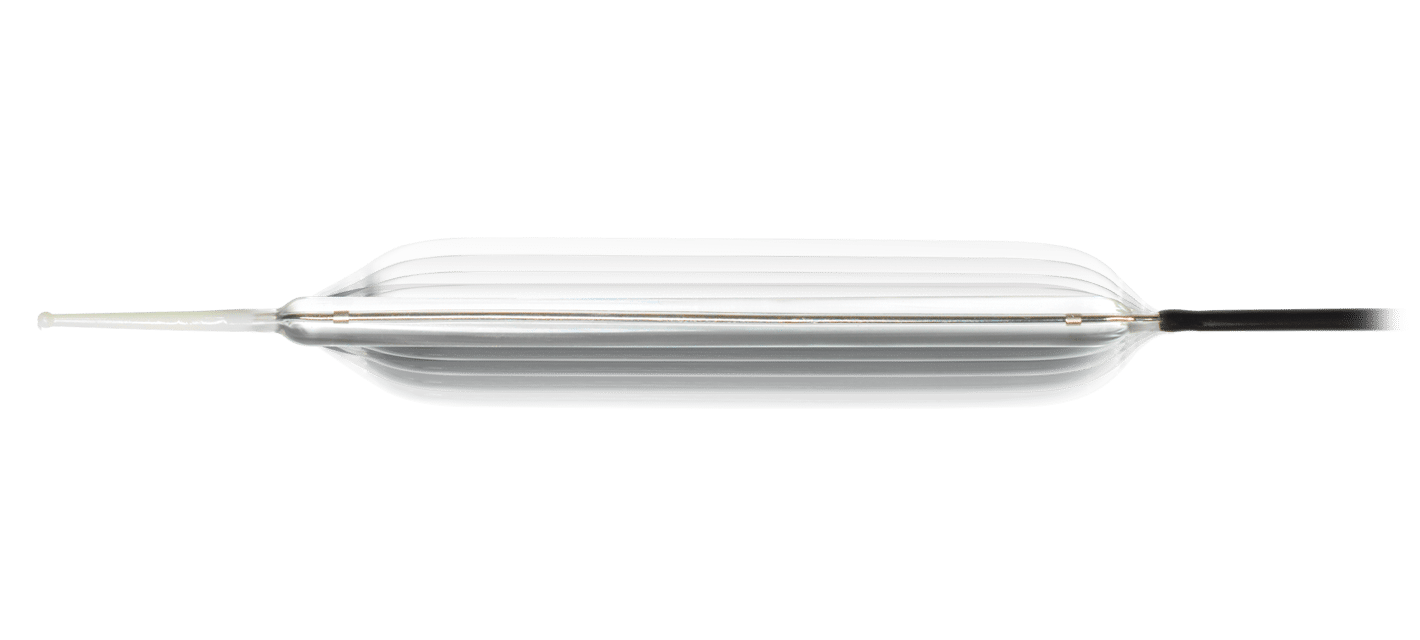
Merit Medical Endotek® Launches New Elation5™ Balloon Dilator
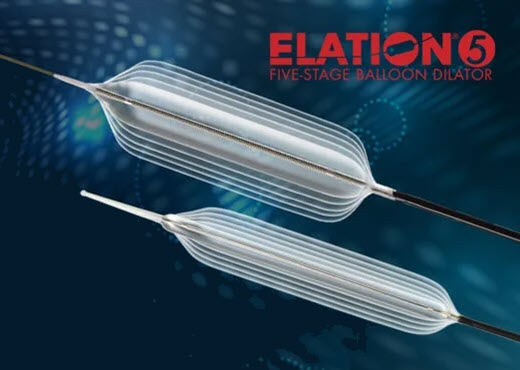
Several key features set Elation5 apart from its 3-stage counterparts. Elation5 has an additional specified diameter on both sides of the standard range of other multi-stage balloons and is available in unique sizes ranging from 5 mm to 21 mm in diameter. The added diameter range of each Elation5 balloon catheter increases clinical utility by reducing the occurrence of using multiple balloons to achieve effective dilation, thus reducing cost and improving efficiency. Like Merit’s flagship Elation® 3-Stage Balloons, Elation5 offers crystal clear endoscopic visualization, quick and complete deflation, a kink-resistant catheter that facilitates multiple scope reinsertions, and a novel catheter securement clip.
KEY FEATURES
Broadest Diameter Range on a Single Catheter – Improves clinical efficiency and reduces cost while simplifying inventory management by stocking fewer SKUs.
Unique 5-mm and 21-mm Balloon Diameters – Expands clinical utility in challenging cases.
Precise, Repeatable Inflation Accuracy – Elation5 Balloons are rigorously tested to ensure optimal performance.
Crystal Clear Endoscopic Visualization – Squared proximal balloon shoulders provide improved optical coupling.
Quick and Complete Deflation – Incomplete deflation can result in wasted time and expense. Paired with Merit’s BIG60® Inflation Device, physicians can count on a best-in-class dilation system.
First and only 5-stage balloons on the market

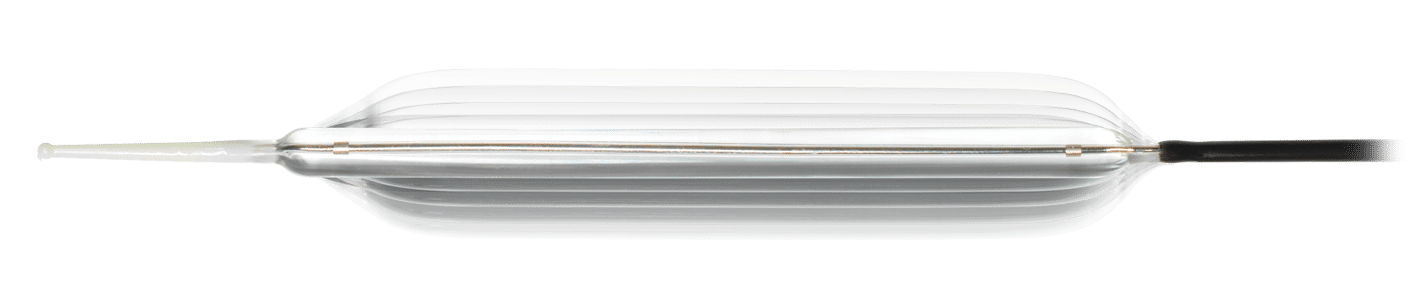
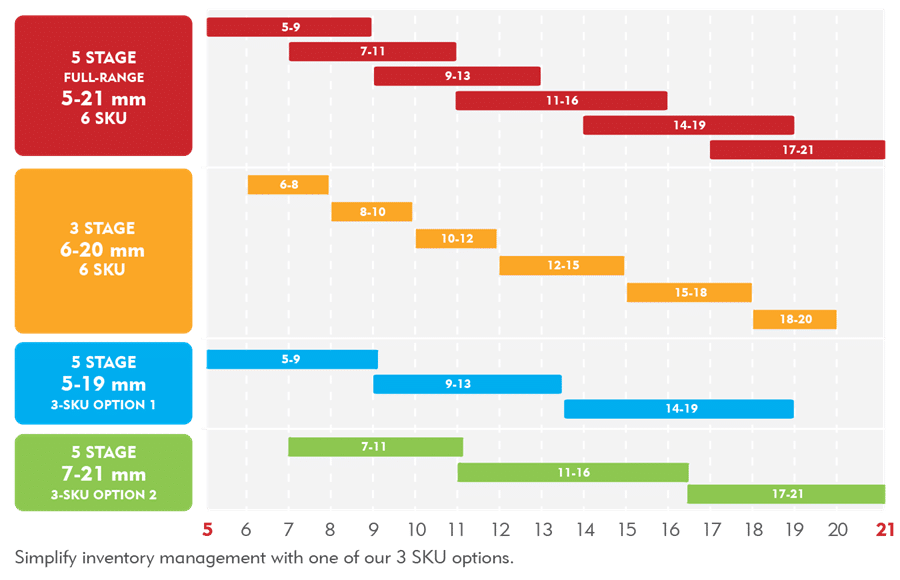
Simplify inventory management while saving money and enhancing clinical efficiency
Broad diameter range and unique diameter sizes increase clinical efficiency, reduce costs, and enhance clinical utility.

Elation5 is an exciting addition to the Merit Endotek portfolio and one that demonstrates Merit’s on-going commitment to understanding customer needs and delivering continuous innovation. In a time when everyone has been asked to do more with less, Elation5 sets the bar for what you should expect in a multi-stage dilation balloon.
Learn more about the Elation5 Dilation Balloon by exploring its product page or by connecting with our Customer Support Center to see how you can incorporate it and other Merit solutions into your practice today.
RELATED PRODUCTS
Merit Recognizes National Osteoporosis Month

Vertebral compression fractures, or VCFs, are the most common osteoporotic fracture—almost twice as common as other fractures caused by osteoporosis. Osteoporotic fractures can lead to long-term pain and even be life threatening.
1 in 3 Women & 1 in 5 Men Over 50 Years Old
To help care for this patient population, we provide a wide range of innovative tools for vertebral augmentation (kyphoplasty) and vertebroplasty treatments.
Listen in as Mrs. Steiner, a patient who suffered from a painful VCF, explains in her own words how treatment with Merit’s steerable Arcadia™ Balloon-Assisted Vertebral Augmentation System helped her resume an active lifestyle.
Browse helpful osteoporosis month resources:
- American Bone Health
- Bone Talk Podcast
- International Osteoporosis Foundation
- National Osteoporosis Foundation
- NIH Osteoporosis and Related Bone Diseases National Resource Center
RELATED PRODUCTS
Before using any of the Merit products mentioned above, refer to Instructions for Use for indications, contraindications, warnings, precautions, and directions for use.
Merit Medical to Exhibit at Virtual ASBrS 2021: Products and Symposia You Won’t Want to Miss

We look forward to connecting with you virtually and encourage you to visit the Merit virtual booth to learn of our latest product platform enhancements and clinical updates.
We are also sponsoring a very compelling industry symposium and two learning sessions, all featuring key opinion leaders and experts in breast cancer care. Mark your calendars to include these products and symposia you won’t want to miss:
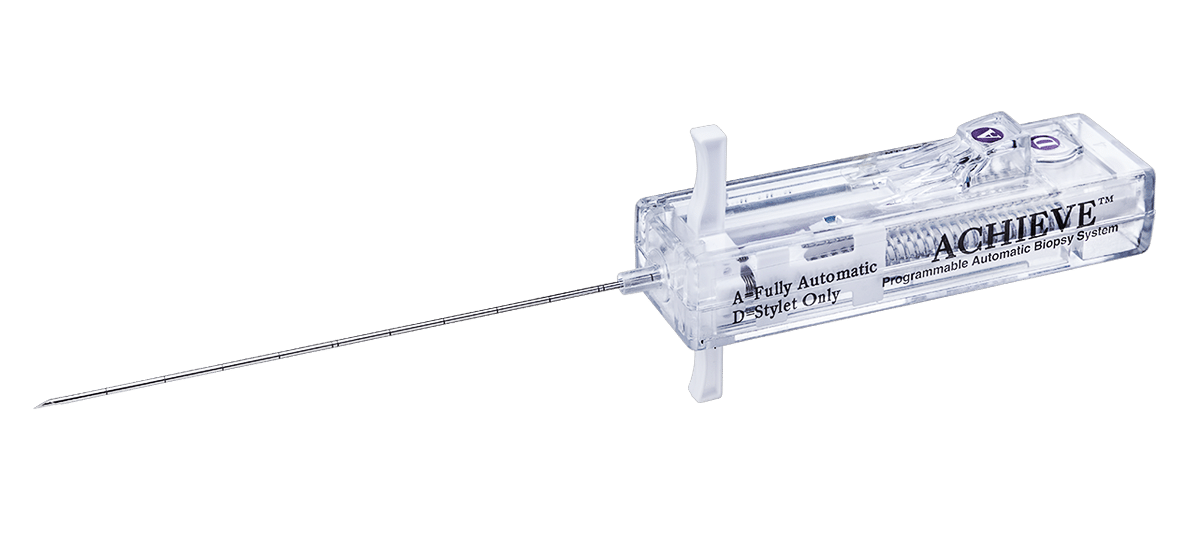
PRODUCTS
As a provider of world-class solutions for the diagnosis, localization, and treatment of cancer, Merit Oncology consistently invests in improving technologies and innovating new platforms to meet physicians’ needs.
SCOUT® RADAR LOCALIZATION

Explore clinical data and hear why physicians choose SCOUT.
SAVI® BRACHY
ACHIEVE® PROGRAMMABLE AUTOMATIC BIOPSY SYSTEM
SYMPOSIA
ASBrS Breakfast Symposium

The Preferred Localization Solution to Treat More Patients: SCOUT
Friday, April 30, 2021
9:00 am – 10:00 am EDT
Description:
SCOUT Radar Localization exclusively spans the care continuum from time of biopsy placement and targeted axillary dissection to excellent surgical outcomes. Discover the state-of-the art localization techniques practiced by key opinion leaders from Cleveland Clinic, Columbia University, University of Colorado, Intermountain Healthcare, and the Advocate System.
Learning Sessions

The Pathway to Market Leadership and the Future of Radar Localization
Includes physician education recording with Michelle Carpenter, MD
Friday, April 30, 2021
2:45 pm – 3:15 pm EDT
Description:
At the time of the 2021 ASBrS meeting, SCOUT will have achieved an important milestone—200K procedures, far exceeding any other wire-free technology.
Join David Gilstrap, Director of Global Product Management at Merit, to learn more about what differentiates radar localization and what is on the horizon for platform enhancements. His presentation will include a physician education recording with Michele Carpenter, MD.

Start-to-Finish APBI in 2 Days: Three-Fraction Treatment with SAVI
Saturday, May 1, 2021
9:15 am – 9:4 5am EDT
Description:
Interested in learning about three-fraction APBI with SAVI? Listen to UC San Diego’s Cate Yashar, MD, and Dan Scanderbeg, PhD, as they discuss outcomes of the TRIUMPH-T Trial, provide an assessment on patient satisfaction, and discuss adopting a three-fraction TRIUMPH-T protocol in your practice.
At Merit, our goal is to lessen the burden cancer places on patients and their loved ones by offering products and services that make this possible. We look forward to seeing you at virtual ASBrS 2021!
*Before using any of the Merit products mentioned above, refer to Instructions for Use for indications, contraindications, warnings, precautions, and directions for use.
REFERENCES
- Khan AJ et al. 2019. “Three-Fraction Accelerated Partial Breast Irradiation (APBI) Delivered With Brachytherapy Applicators Is Feasible and Safe: First Results From the TRIUMPH-T Trial.” Int J Radiat Oncol Biol Phys 104, no. 1:67– PMID: 30611839.
Merit Medical ISO Certified for Environmental Sustainability and Employee Safety

To help guide us, our facilities worldwide use a set of international standards created by ISO (International Organization of Standardization)—an independent, non-governmental global group that develops guidelines for companies like Merit to use to help ensure quality, efficiency, and safety of its products, services, and systems.
There are many different ISO certifications, each with separate standards and criteria to follow. No matter the focus, ISO certification means that a system, protocol, service, or procedure has met all the requirements for that specific standardization.
The following is a breakdown of the ISO certifications within our sustainability program that our facilities have received as well as our goals for 2021–2022:
ISO 14001: ENVIRONMENTAL MANAGEMENT SYSTEMS
ISO 14001 is the international standard for certifying an environmental management system (EMS) to enhance environmental performance. Merit’s EMS has several components, for example the practices, policies, goals, legal requirements, and progress monitoring that enable us to reduce our environmental impact and increase operating efficiency. ISO 14001 standards have helped guide our company in developing the EMS for each of our manufacturing facilities.
Merit Facilities with ISO 14001 Certification
ISO Goal
All Merit manufacturing facilities will be ISO 14001 certified by the end of 2021.
Currently, the following Merit facilities are pursuing certification:
ISO 45001: Occupational Health and Safety Management Systems
ISO 45001 guides businesses in standardizing their Occupational Health & Safety (OH&S) management system to continuously seek reduction in occupational injuries and/or diseases including promoting and protecting physical and mental health. Merit’s goal to obtain certification of its OH&S system is the next step in maintaining and improving our top priority to provide a healthy and safe workplace by controlling factors that could lead to injury or illness.
ISO Goal
All Merit manufacturing facilities will be ISO 45001 certified by the end of 2022.
At this time, the following Merit facilities are pursuing certification:
ISO 50001: Energy Management Systems
ISO 50001 standards provide businesses with guidance for improving energy conservation by developing an energy management system (EnMS). Much like the aforementioned EMS, an EnMS incorporates energy management into business practices and policies, enabling companies to better manage their energy use, conserve resources, and improve energy performance.
Merit Facilities with ISO 50001 Certification
ISO Goal
All Merit manufacturing facilities will have or be pursuing ISO 50001 certification by the end of 2022.
At this time, the following Merit facilities are already pursuing certification:
We understand and recognize our responsibility as a good corporate citizen. By pursuing continuous improvement through ISO standardization, we reaffirm our commitment to building a sustainable world for our business, our future, and our communities.
We wish everyone a Happy Earth Day 2021!
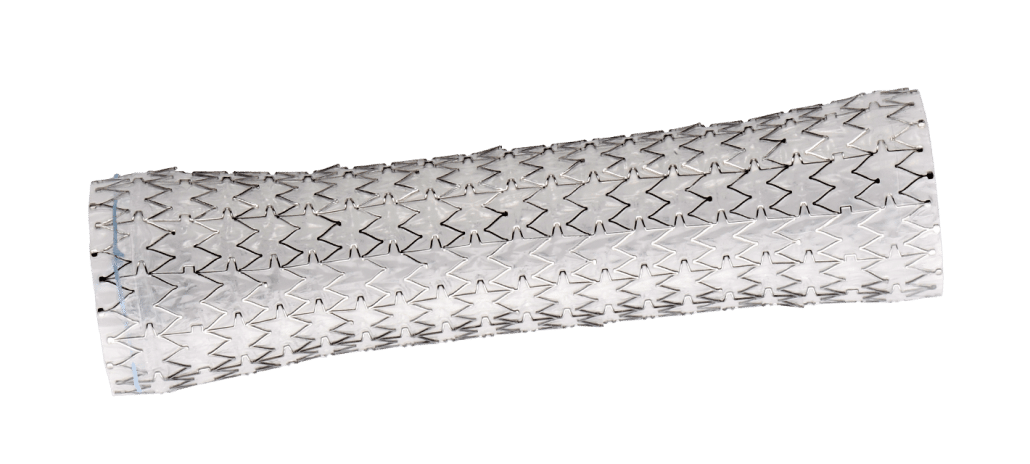
Addressing Complications of Esophageal Stenting with the EndoMAXX® Stent
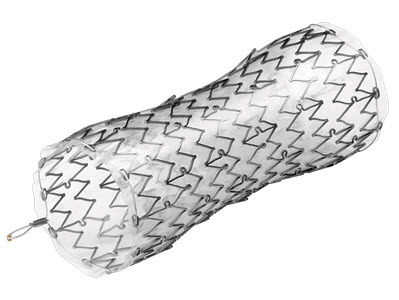
There are numerous treatment options available to help in the palliation of a malignant esophageal obstruction, such as photodynamic therapy, thermal ablative techniques, surgical resection or bypass, and chemotherapy/radiotherapy. However, endoscopic stenting offers significant advantages over these other therapies, as stents are generally easy and quick to place. They are safe, have a good complication profile, and are well-tolerated with a low incidence of significant pain.1,2
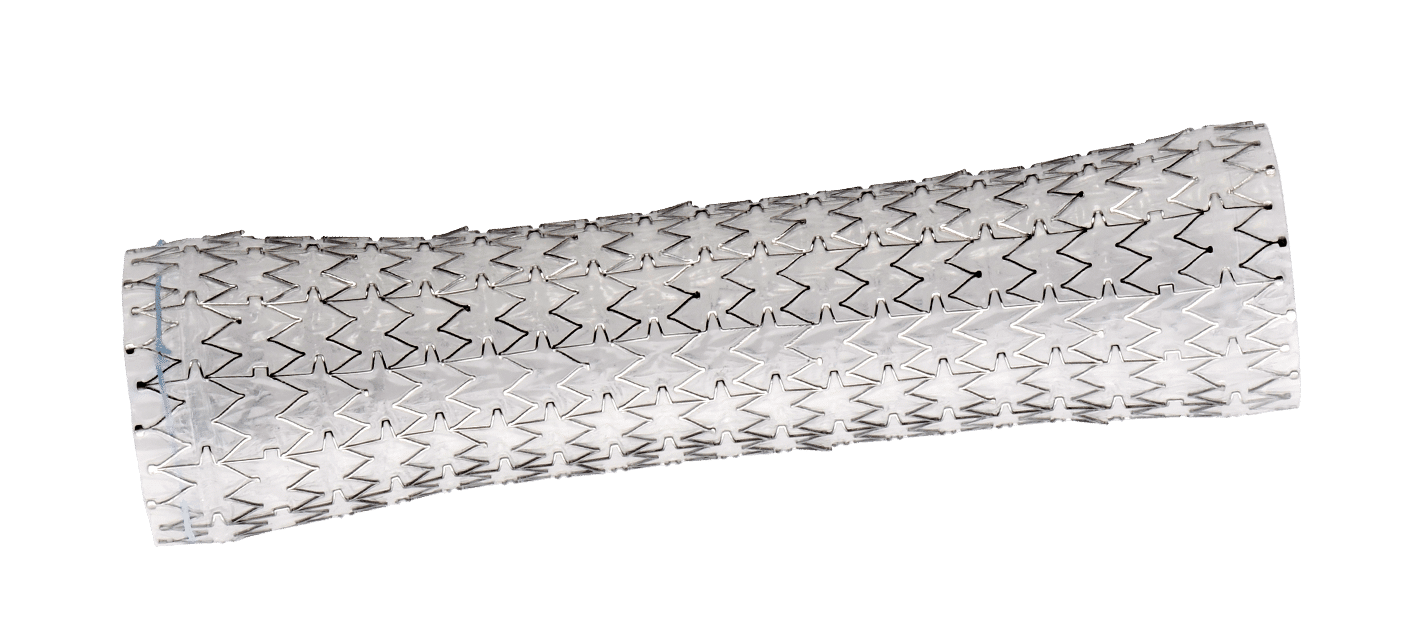
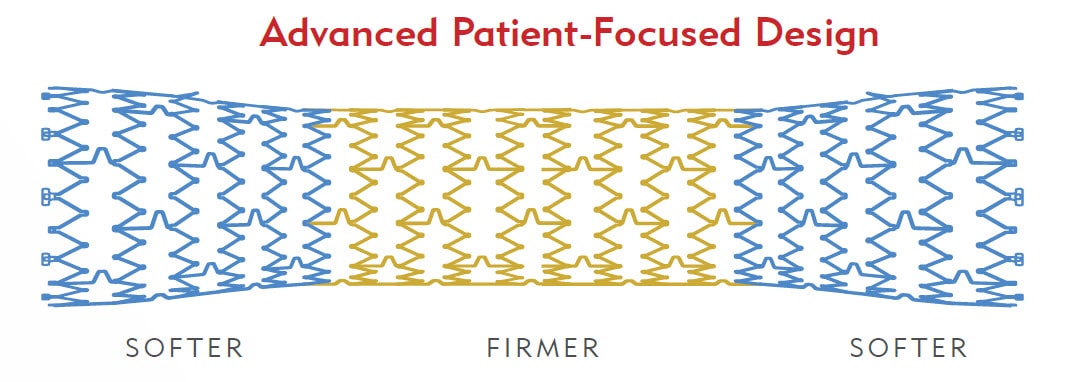
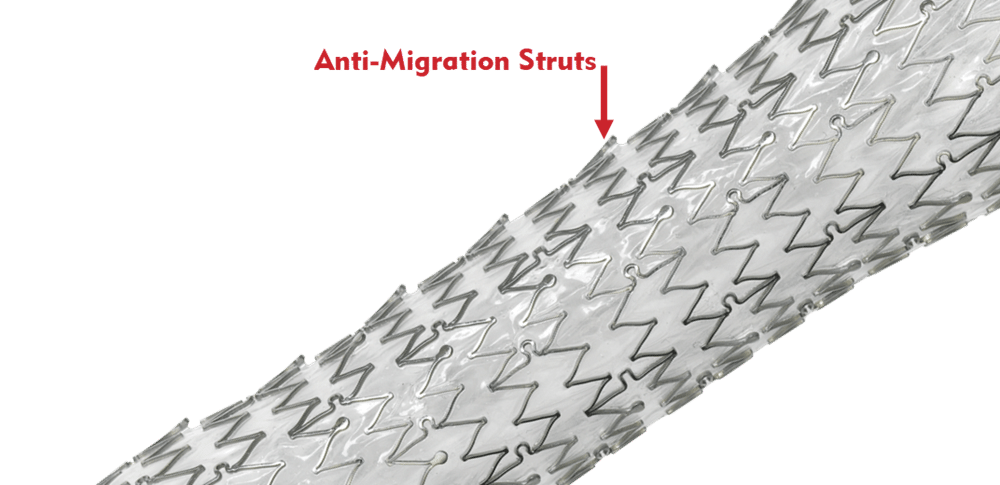
Despite having a good complication profile, two common complications of esophageal stenting exist: chest pain and stent migration. The EndoMAXX is designed to address each.
Chest pain due to esophageal stent placement has incidence rates ranging from 12%3 to as high as 37%.4 This pain is typically due to the expansion force, or outward pressure, an esophageal stent exerts on esophageal tissue, a tumor, or a stricture when implanted. It is believed that this force directly corresponds to the discomfort the patient feels while the stent is in place. Clinical guidance also suggests this force may contribute to perforation, a life-threatening additional complication that can occur with an esophageal stent.
The expansion force of the EndoMAXX is 2.4 N, compared to 5.4 N of the market-leading esophageal stent in the US.5 In addition, the EndoMAXX stent is designed with 2.5 cm of flare at each end of the stent. This feature helps anchor the stent within the esophageal lumen. Soft flared ends and a firm mid-body help to dilate an obstruction while protecting healthy esophageal mucosa.
Beyond having a lower radial force, the laser-cut design of the EndoMAXX has virtually no foreshortening or elongation of the stent during deployment, allowing for accurate sizing to the patient’s anatomy. A recent study published by Essrani et al. in Cureus Journal of Medical Science confirmed that “[t]he most common complication . . . encountered was chest pain, which was transient and mostly resolved without any intervention.”2
In addition, a study by Dua et al. published in Gastrointestinal Endoscopy showed that “[c]hest pain was reported in 11% of patients, and in two-thirds of these cases chest pain developed several weeks after stent placement while the patients were receiving radiotherapy.” The authors concluded that “[t]he relatively low incidence of chest pain in this series could be related to the use of smallest-diameter (19 mm) stents in all patients with strictures.”1
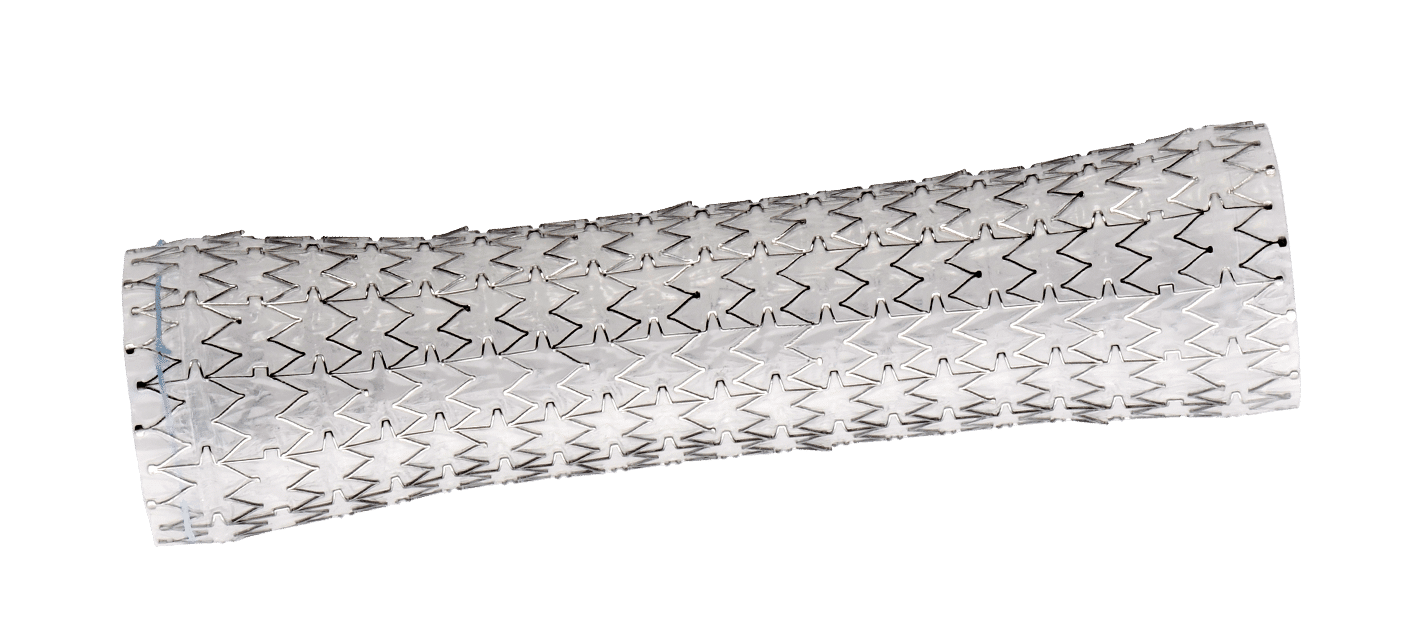
Migration is also a common complication of esophageal stent placement. Research shows migration rates for self-expanding metal stents range from 23 % to 31 % in malignant strictures. 6-8 In an effort to reduce migration, the EndoMAXX stent is designed with proprietary anti-migration struts that provide increased mucosal wall contact and friction.
The EndoMAXX is designed with both proximal and distal metal sutures to provide a means for repositioning of the stent post placement and removal if necessary. This can be accomplished by using rat-tooth forceps and grasping the gold metal bead in the suture loop at the proximal end of the stent. Then carefully, using a purse-string effect, the proximal end of the stent is released from contact with the esophageal wall and traction is applied as it is removed.
No surgery is free of complications, but choosing products designed to decrease their incidence may result in better patient outcomes. Merit’s esophageal stents have a number of key features that address common concerns associated with esophageal stent placement, all while maintaining luminal patency.
For more information regarding esophageal stenting solutions, visit our GI Stricture Management page, the EndoMAXX product page, or connect with our Customer Support Center.
References
- Dua K et al. 2014. “Efficacy and Safety of a New Fully Covered Self-Expandable Non-Foreshortening Metal Esophageal Stent.” Gastrointestinal Endoscopy 80, no. 4 (Oct): 577–585. PMID: 24685007.
- Essrani R et al. 2020. “Complications Related to Esophageal Stent (Boston Scientific Wallflex vs. Merit Medical Endotek) Use in Benign and Malignant Conditions.” Cureus Journal of Medical Science12, no. 3 (Mar 23): e7380. PMID: 32328390.
- Hindy P et al. 2012. “A Comprehensive Review of Esophageal Stents.” Gastroenterol Hepatol (NY) 8, no. 8 (Aug): 526–534. PMID 23293566.
- van Boeckel P et al. 2010. “A New Partially Covered Metal Stent for Palliation of Malignant Dysphagia: A Prospective Follow-up Study.” Gastrointest Endosc 72, no. 6: 1269–1273. PMID: 20951988.
- Data on File.
- Siddiqui A et al. 2012. “Placement of Fully Covered Self-Expandable Metal Stents in Patients with Locally Advanced Esophageal Cancer Before Neoadjuvant Therapy.” Gastrointestinal Endosc 76, no. 1 (Jul): 44–51. PMID: 22726465.
- Martinez J et al. 2011. “Esophageal Stenting in the Setting of Malignancy.” ISRN Gastroenterology 2011: 719575. PMID: 21991527.
- Shenfine J et al. 2005. “A Pragmatic Randomized Controlled Trial of the Cost-Effectiveness of Palliative Therapies for Patients with Inoperable Esophageal Cancer.” Health Teach Assess 9, no. 5 (Feb): 1–121. PMID: 15717937.
Helping You Understand Esophageal Cancer

Across the nation, Americans are recognizing April as Esophageal Cancer Awareness Month—a full 30 days dedicated to learning more about the disease, signs and symptoms of it, and steps individuals can take to reduce their risk.
This year alone, it’s estimated there will be more than 19,000 new esophageal cancer cases diagnosed and more than 15,000 deaths from the disease in the United States.
To help this patient population, our goal at Merit Medical is to not only provide the tools physicians need to treat and improve outcomes for individuals with esophageal cancer but also share knowledge and increase awareness surrounding the disease.
Use the following infographics and resources to inform yourself and prepare for a discussion with your doctor about your own personal risk.
WHAT IS ESOPHAGEAL CANCER?

Esophageal cancer is cancer found in the esophagus—the hollow, muscular tube in your body that carries food and liquid from the throat to the stomach.
ESOPHAGEAL CANCER RISK FACTORS
Although a rare condition, esophageal cancer has an average five-year survival rate of approximately 20%.
Risk factors for developing esophageal cancer include the following:




If you’re experiencing heartburn that’s severe or frequent, it’s important you talk with your doctor. The longer it continues, it can damage the inner lining of the esophagus, leading to a condition called Barrett’s esophagus, which increases your risk of esophageal cancer.
Find help to stop smoking and support to reduce alcohol consumption.
Learn more about other risk factors, including how men are three times as likely as women to suffer from esophageal cancer.
MOST COMMON TYPES OF ESOPHAGEAL CANCER
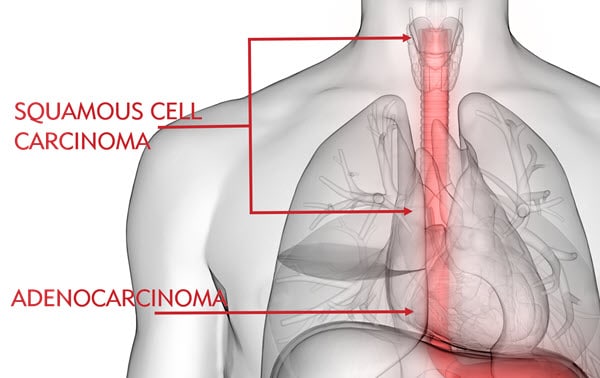
Esophageal cancer is most common in two forms: squamous cell carcinoma and adenocarcinoma. Squamous cell carcinoma typically affects the upper and middle esophagus, whereas adenocarcinoma is commonly found in the lower esophagus near the stomach and is believed to be related to stomach acid exposure. Learn about other forms of esophageal cancer.
Adenocarcinoma is the most common type of esophageal cancer among Caucasian people, whereas squamous cell carcinoma is more common among African Americans. In comparison, American Indian/Alaska Natives, Hispanics, and Asians/Pacific Islanders have lower rates of esophageal cancer, respectively.
SIGNS & SYMPTOMS
Esophageal cancer can be difficult to treat because individuals don’t usually experience symptoms until the disease is advanced. Esophageal cancer usually doesn’t cause symptoms in its early stages.
As it progresses, symptoms can include:
- Difficulty swallowing, can be painful
- Hoarse voice
- Indigestion or heartburn
- Weight loss
- Persistent cough
- Vomiting
Some risk factors for esophageal cancer can’t be avoided, such as genetics or age. However, there are many lifestyle changes that can help you reduce your risk, such as avoiding tobacco and treating acid reflux:

DIAGNOSIS & TREATMENT
If you’ve been diagnosed with esophageal cancer, you most likely have many questions. You also have multiple treatment options. Your cancer care team will discuss each with you, helping you make the best decision for you.
Learn more about esophageal cancer diagnosis, treatment, and life after treatment or visit the Esophageal Cancer Action Network (ECAN) for a free patient guide.
MORE RESOURCES
- American Association for Cancer Research
- American Cancer Society
- Cancer Care
- Cancer Support Community
- Esophageal Cancer Awareness Association
- ECAN
- National Cancer Institute
- National Foundation for Cancer Research
RELATED PRODUCTS
Merit 2020 Garden Accomplishments

At Merit Medical, we’re dedicated to reducing our environmental footprint. That’s why we take steps at each of our facilities to create a culture of innovation that lessens our impact on the world around us. A prime example of how we achieve this can be seen at our Salt Lake City facility, where we have established a community garden that provides farm-to-table nutrition for employees and the facility café.
As we head into Spring—and begin the 2021 garden season—we’d like to take a moment to reflect on all the Merit Community Garden accomplished in 2020.
EMPLOYEE PARTICIPATION
45 Departments
About 160 employees participated in growing their own produce in an assigned garden box at the Merit community garden, representing 45 different departments. One-third of gardeners participated for the first time.
300 Visits
Nearly 150 employees, from 52 departments across Merit, visited the U-Pick portion of the garden, where they could exchange weeding and cultivating services for a basket of fresh produce, totaling almost 300 visits.
3000 Pounds
More than 3,000 pounds of produce was distributed to U-Pick participants.
HOMEGROWN GOODNESS

Approximately 9,000 plants were grown in the Merit greenhouse, 4,000 of which were purchased by employees.
Cut flower orders doubled in 2020, with 160 arrangements prepared for employees.
A total of 1,600 plants were grown for the Merit Salt Lake City landscaping department.
FARM-TO-TABLE NUTRITION

Although most of the café produce was diverted to the U-Pick section in 2020, the garden still provided almost 400 pounds of produce to the Merit Café.
WASTE REDUCTION

Six tons of green waste was taken to the Trans-Jordan Landfill to make compost.
GIVING BACK

Plant sales raised $13,000 for the Candy Cane Program to help those in need during the holiday season.

Nearly 300 pounds of produce was donated to low-income senior centers.

All inedible produce was donated to farm animals at Roots Charter School, a nonprofit alternative high school in Salt Lake City.
We thank the Merit Community Garden Project team for making 2020 such a success, and we look forward to an even greener 2021 garden season!
Learn more about the Merit Community Garden.
See what the Merit Community Garden is up to by following them on Facebook.
Merit Medical to Exhibit New Products and Must-See Educational Symposia During SIR 2021

Merit will be exhibiting at this year’s Society of Interventional Radiology (SIR) meeting held virtually from March 20-26. At the Merit virtual booth, we will showcase several innovative products—including the newly launched SplashWire™ Hydrophilic Steerable Guide Wire—and hold two must-see educational symposia.
Mark your calendars for the following events at our virtual booth:
March 20, Saturday
Calling all medical students, nurse practitioners, physician assistants, and residents! This is your chance to learn about our renowned Think Education program. Designed and taught by physicians, Think Education offers both training and clinical support needed to implement new tools and techniques into your practice. Explore upcoming courses.
March 21, Sunday
A day we dedicate to recognizing all the incredible women who work in interventional radiology and make a difference in patients’ lives each day.

March 22, Monday
Have you met our latest guide wire? Stop by the Merit virtual booth to get a close-up of the SplashWire, designed to deliver superior performance in diagnostic and interventional procedures. See how it can help you traverse difficult lesions and support clinical outcomes in the most challenging procedures. Learn more about the new SplashWire.
March 23, Tuesday
Familiarize yourself with the CorVocet, a biopsy system designed to cut a full core of tissue, providing large specimens for pathological examination. With a lightweight and ergonomic design, the CorVocet facilitates one-handed priming, positioning, and deployment, which can be beneficial during image-guided procedures. Discover the CorVocet.

March 24, Wednesday
Stop by and learn about the Resolve ConvertX, a stent system used for temporary internal drainage in patients with ureteral or biliary obstructions. Learn how its technology provides a less invasive option by eliminating the need for a second interventional procedure. Explore the ConvertX.
SYMPOSIUM: Management of Venous Access in Patients with Central Venous Occlusions: Surfacer® Inside-Out® Access Catheter System
DATE: Thursday, March 25
SPEAKER: Mahmood K. Razavi, MD
TIME: 7:10-7:50 pm ET
About the Product:
The Surfacer is a unique access catheter system designed to obtain right-sided central venous access in patients with venous obstructions. Learn more and watch how the Surfacer works here.
SYMPOSIUM: Arcadia™: Next Generation Balloon-Assisted Vertebral Augmentation

DATE: Friday, March 26
SPEAKERS:David Shelley, MD
Douglas P. Beall, MD
Scott A. Koss, MD
TIME: 7:10-7:50 pm ET
About the Product:
Harnessing Merit Spine’s unique portfolio feature of steerability, the Arcadia is an intuitive balloon-assisted vertebral augmentation (kyphoplasty) system that allows for a bipedicular footprint through a unipedicular approach, offering several benefits when treating patients with painful benign or pathologic vertebral compression fractures. Learn more here.

 Designing an Environmental Management System
Designing an Environmental Management System